Information Site About Reproductive System
About Me
Blog Archive
-
▼
2009
(58)
-
▼
December
(17)
- Syphilis During Pregnancy
- STDs and Pregnancy - Fact Sheet
- URINARY TRACT INFECTIONS in PREGNANCY
- GROUP B STREPTOCOCCUS INFECTION and PREGNANCY
- SWINE FLU and PREGNANCY
- GENITAL HERPES IN PREGNANCY
- LISTERIA and PREGNANCY
- REPIRATORY INFECTIONS DURING PREGNANCY
- HEPATITIS IN PREGNANCY
- CYTOMEGALOVIRUS
- CHLAMYDIA
- RUBELLA
- TOXOPLASMOSIS
- RECTOCELE
- CYSTOCELE
- PROLAPSE OF THE UTERUS
- PELVIC FLOOR
-
▼
December
(17)
Friday, December 4, 2009
What is syphilis?
Syphilis is a sexually transmitted infection (STI) that's caused by a type of bacterium called a spirochete. If left untreated, syphilis can have very serious short- and long-term consequences. Fortunately, with timely antibiotic treatment, these consequences can usually be avoided.
Syphilis is transmitted by direct contact with a sore on an infected person. The most common way to get syphilis is through vaginal, anal, or oral sex, but it's also possible to get it by kissing someone with a syphilitic sore on or around the lips or in the mouth or by exposing an area of broken skin to a sore.
Syphilis can be transmitted to your baby through the placenta during pregnancy or by contact with a sore during birth.
The infection is relatively rare among women in the United States, with 1.1 cases per 100,000 women in 2007, but that number was up 10 percent from 2006. The rates are significantly higher in communities with high levels of poverty, low levels of education, and inadequate access to health care.
The number of babies in the United States born with syphilis also rose – after 14 years of decline – from 339 new cases in 2005 to 382 cases in 2006 to 430 cases in 2007.
What are the symptoms?

In the first stage, known as primary syphilis, the characteristic symptom is a painless and highly infectious sore (or sores) with raised edges called a CHANCRE. The chancre shows up at the site of infection, usually about three weeks after you're exposed to the bacteria, though it may appear earlier or up to three months later.
Because the chancre may be inside your vagina or your mouth, you might never see it. A chancre could also show up on your labia, perineum, anus, or lips, and your lymph nodes may be enlarged in the area where the sore develops.
If you get appropriate treatment at this stage, the infection can be cured. If you're not treated, the sore lasts three to six weeks and then heals by itself. However, the spirochetes are likely to continue to multiply and spread throughout the bloodstream. When this happens, the disease progresses to the next stage, called secondary syphilis.
In the secondary stage, syphilis can have a variety of symptoms that show up in the weeks or months after the sore first appeared, but again, they might not be noticeable.

Without treatment, the symptoms generally clear up on their own within a few months, but the infection stays in your body. The bacteria continue to multiply during this latent phase and can cause very serious problems years later.
In fact, about 1 in 3 people who don't get proper treatment will progress to what's called tertiary syphilis. This late stage of the disease can develop up to 30 years after you were first infected and can cause serious heart abnormalities. Damaging and potentially lethal lesions can develop in your bones, on your skin, and in a host of organs. Fortunately, most people get treated early enough these days that very few end up with tertiary syphilis.
Syphilis can also infect your central nervous system – your brain and spinal cord. This is called neurosyphilis, and it can occur at any stage of the disease. Early on, it may cause problems like meningitis.
Late neurosyphilis can lead to seizures, blindness, hearing loss, dementia, psychosis, spinal cord problems, and eventually death.
How can syphilis affect my pregnancy and my baby's health?

If you don't get treated, there's a very high chance that your baby will be infected, particularly if you're in the early stages of the disease, when it's most infectious. About 40 percent of pregnant women with untreated early syphilis end up having a miscarriage, a stillbirth, or a baby who dies soon after birth. Syphilis also increases the risk of preterm birth and intrauterine growth restriction.
Some babies infected with syphilis whose mothers are not treated in a timely fashion during pregnancy develop problems before birth that are visible on an ultrasound. These problems might include an overly large placenta, fluid in their abdomen and severe swelling, and an enlarged liver or spleen.
An infected baby may have other abnormalities at birth, such as a skin rash and lesions around the mouth, genitals, and anus; abnormal nasal secretions; swollen lymph glands; pneumonia; and anemia.
Most babies don't have these symptoms initially, but without treatment they develop some symptoms within the first month or two after birth. And whether or not there are obvious symptoms early on, if the disease isn't treated, babies born with syphilis may end up with more problems years later, such as bone and teeth deformities, vision and hearing loss, and other serious neurological problems.
That's why it's critical for women to be tested and treated during pregnancy, and for any baby who may have syphilis at birth to be fully evaluated and treated as well.
Will I be tested for syphilis during my pregnancy?
Yes. Even though the infection is relatively rare, it's considered vitally important to detect and treat syphilis during pregnancy. The CDC recommends that all pregnant women be screened for the infection at their first prenatal visit, and some states require that all women be tested again at delivery.
If you live in a community where syphilis is prevalent or you're otherwise at high risk, you should be tested again at 28 weeks and at delivery. You'll also be retested for syphilis if you've contracted another STI during your pregnancy or if you or your partner develops symptoms of syphilis.
Because it takes about four to six weeks after exposure to get a positive result from the blood test, the result may be negative if you're tested too soon.
So if you had high-risk sex a few weeks before your test or your partner recently had symptoms, tell your practitioner so you can be tested again in a month. If your screening test is positive, the lab will perform a more specific test on your blood sample to tell for sure whether you have syphilis.
Having syphilis makes you more susceptible to HIV if you're exposed to it, so if you test positive for syphilis, you should also be tested (or retested) for HIV and other STIs.
And if you have primary syphilis, you'll need to be tested for HIV again in three months
How is syphilis treated during pregnancy?
Penicillin is the only antibiotic that's both safe to take during pregnancy and able to successfully treat both mother and baby for syphilis. If you have syphilis, you'll get treated with one or more injections of penicillin, depending on the stage of the disease and whether you have neurosyphilis. (If you have any symptoms of neurosyphilis, you'll have a spinal tap to check for it.) If you're allergic to penicillin, you'll need to be desensitized to the drug first, so you can receive it.
In many pregnant women, treatment for syphilis causes a temporary reaction that may include fever, chills, headache, and muscle and joint aches. These symptoms tend to appear several hours after treatment and go away on their own in 24 to 36 hours.
The treatment may also cause some changes in your baby's heart rate, and if you're in the second half of your pregnancy, it may cause contractions. (If you notice any contractions or a decrease in fetal movement, you should call your caregiver immediately. In some cases, your caregiver may opt to treat you in the hospital so you can be monitored.)
Your partner will also need to be tested, and he'll be treated if he's positive or has had sexual contact with you in the last three months, even if his blood test is negative. You need to refrain from sexual contact until both of you have been treated. After treatment, you'll have regular blood tests to make sure the infection has cleared and you haven't been reinfected, and you'll have an ultrasound to check on your baby.
How can I avoid getting syphilis?
Have sex only with a partner who has sex only with you and has tested negative for syphilis. While condoms can prevent transmission of HIV and other STIs, they only offer protection from syphilis if the sore is on your partner's penis – they won't protect you from sores that aren't covered by the condom.
Remember, too, that you can get syphilis if a partner's sore touches any of your mucous membranes (such as in your mouth or vagina) or broken skin (a cut or scrape).
If you've had syphilis once, that doesn't mean you can't get it again. You can become reinfected.
If there's a possibility that you've been exposed to syphilis or any other STI during pregnancy, or you or your partner has any symptoms, tell your practitioner right away so you can be tested and treated if necessary.
Can Pregnant Women Become Infected With STDs
Yes, women who are pregnant can become infected with the same sexually transmitted diseases (STDs) as women who are not pregnant. Pregnancy does not provide women or their babies any protection against STDs. The consequences of an STD can be significantly more serious, even life threatening, for a woman and her baby if the woman becomes infected with an STD while pregnant. It is important that women be aware of the harmful effects of STDs and knows how to protect themselves and their children against infection.
How Common Are STDs In Pregnant Women
Some STDs, such as genital herpes and bacterial vaginosis, are quite common in pregnant women in the United States. Other STDs, notably HIV and syphilis, are much less common in pregnant women. The table below shows the estimated number of pregnant women in the United States who are infected with specific STDs each year.
| STDs | Estimated Number Of Pregnant Women |
| Bacterial Vaginosis | 1.080.000 |
| Herpes Simplex Virus 2 | 880-.000 |
| Chlamydia | 100.000 |
| Trichomoniasis | 124.000 |
| Gonorrhoea | 13,200 |
| Hepatitis B | 16.000 |
| HIV | 6.400 |
| Syphilis | < 1.000 |
How Do STDs Affect A Pregnant Women and Her Baby
STDs can have many of the same consequences for pregnant women as women who are not pregnant. STDs can cause cervical and other cancers, chronic hepatitis, pelvic inflammatory disease, infertility, and other complications. Many STDs in women are silent; that is, without signs or symptoms.
STDs can be passed from a pregnant woman to the baby before, during, or after the baby’s birth. Some STDs (like syphilis) cross the placenta and infect the baby while it is in the uterus (womb). Other STDs (like gonorrhea, chlamydia, hepatitis B, and genital herpes) can be transmitted from the mother to the baby during delivery as the baby passes through the birth canal. HIV can cross the placenta during pregnancy, infect the baby during the birth process, and unlike most other STDs, can infect the baby through breastfeeding.
A pregnant woman with an STD may also have early onset of labor, premature rupture of the membranes surrounding the baby in the uterus, and uterine infection after delivery.
The harmful effects of STDs in babies may include stillbirth (a baby that is born dead), low birth weight (less than five pounds), conjunctivitis (eye infection), pneumonia, neonatal sepsis (infection in the baby’s blood stream), neurologic damage, blindness, deafness, acute hepatitis, meningitis, chronic liver disease, and cirrhosis. Most of these problems can be prevented if the mother receives routine prenatal care, which includes screening tests for STDs starting early in pregnancy and repeated close to delivery, if necessary. Other problems can be treated if the infection is found at birth.
Should Pregnant Women Be Tested For STDs ?
Yes, STDs affect women of every socioeconomic and educational level, age, race, ethnicity, and religion. The CDC 2006 Guidelines for Treatment of Sexually Transmitted Diseases recommend that pregnant women be screened on their first prenatal visit for STDs which may include:
In addition, some experts recommend that women who have had a premature delivery in the past be screened and treated for bacterial vaginosis at the first prenatal visit.
Pregnant women should ask their doctors about getting tested for these STDs, since some doctors do not routinely perform these tests. New and increasingly accurate tests continue to become available. Even if a woman has been tested in the past, she should be tested again when she becomes pregnant.
Can STDs Be Treated During Pregnancy ?
Chlamydia, gonorrhea, syphilis, trichomoniasis, and bacterial vaginosis (BV) can be treated and cured with antibiotics during pregnancy. There is no cure for viral STDs, such as genital herpes and HIV, but antiviral medication may be appropriate for pregnant women with herpes and definitely is for those with HIV. For women who have active genital herpes lesions at the time of delivery, a cesarean delivery (C-section) may be performed to protect the newborn against infection. C-section is also an option for some HIV-infected women. Women who test negative for hepatitis B, may receive the hepatitis B vaccine during pregnancy.
How Can Pregnant Women Protect Themselves Against Infection ?
The surest way to avoid transmission of sexually transmitted diseases is to abstain from sexual contact, or to be in a long-term mutually monogamous relationship with a partner who has been tested and is known to be uninfected.
Latex condoms, when used consistently and correctly, are highly effective in preventing transmission of HIV, the virus that causes AIDS. Latex condoms, when used consistently and correctly, can reduce the risk of transmission of gonorrhea, chlamydia, and trichomoniasis Correct and consistent use of latex condoms can reduce the risk of genital herpes, syphilis, and chancroid only when the infected area or site of potential exposure is protected by the condom. Correct and consistent use of latex condoms may reduce the risk for genital human papillomavirus (HPV) and associated diseases (e.g. warts and cervical cancer).
Monday, November 30, 2009
Gonorrhoea
Gonorrhoea is caused by bacteria known as Neisseria gonorrhoeae.
It usually affects the genital area, although the throat or anus (back passage) may also be involved.
Gonorrhoea affects both men and women and is easily transmitted during vaginal intercourse. It can also be transmitted during anal or oral sex.
Gonorrhoea may not cause symptoms in women
A lack of specific signs and symptoms means gonorrhoea may go undetected for longer in women. Often there are no symptoms. Sometimes, gonorrhoea causes:- An unusual discharge from the vagina
- Pain while urinating or passing water.
Untreated gonorrhoea can lead to infertility in women
If left untreated, gonorrhoea can lead to pelvic inflammatory disease (PID), which can cause infertility. Symptoms of PID include:- Lower abdominal pain and tenderness
- Deep pain during sexual intercourse
- Heavy and painful periods
- Fever.
A check for gonorrhoea may be recommended
 Because gonorrhoea may not cause symptoms until PID has already developed, sexually active women who have recently had a change of sexual partner or feel they may be at risk of a sexually transmissible infection (STI) should have a test for gonorrhoea (and for chlamydia infection).
Because gonorrhoea may not cause symptoms until PID has already developed, sexually active women who have recently had a change of sexual partner or feel they may be at risk of a sexually transmissible infection (STI) should have a test for gonorrhoea (and for chlamydia infection).Men may experience a burning sensation while urinating
Gonorrhoea commonly infects the inside of the penis (the urethra). Symptoms may include:
- A burning sensation while urinating or passing water
- A white or yellow pus-like discharge from the penis
- Swelling and pain in the testicles, which can occur if the gonorrhoea infection goes untreated.
Oral and anal gonorrhoea
 In both men and women:
In both men and women: - ANAL GONORRHOEA Anal gonorrhoea often occurs without signs or symptoms
- THROAT GONORRHOEA may cause a sore throat, however, it usually occurs without symptoms.
Gonorrhoea is treated with antibiotics
Gonorrhoea is treated with antibiotics. Some strains of gonorrhoea are now resistant to penicillin and some other antibiotics. Tell your doctor if you have been travelling overseas because many of the new resistant strains have originated from outside Australia.Prevention through the proper use of condoms and dams is best
The best protection against gonorrhoea is to always use barrier protection such as condoms, female condoms and dams (a thin piece of latex placed over the anal or vulval area during oral sex). Condoms and dams can be used for oral-vaginal sex and oral-anal sex to help prevent the spread of infection.
Condoms for men can be bought from supermarkets, chemists and other outlets. Female condoms and dams are available through Family Planning Victoria and may be available from selected shops. Latex free condoms are also available from some outlets. Male condoms and lubricant are available free from the Melbourne Sexual Health Centre, along with female condoms and dams on request.
When using a condom for men you should:
- Open the packet carefully so that you don’t tear the condom.
- Pinch the tip of the condom before carefully rolling it down the entire shaft of the erect penis.
- Do not use spit, Vaseline, baby oil or other oil-based lubricants.
- Use water-based lubricants, such as KY, Muko or Wet Stuff.
- Withdraw the penis before the erection is lost, so that the condom does not fall off. Hold the base of the condom to prevent spills.
- Store condoms in a cool, dry place and check the expiry date.
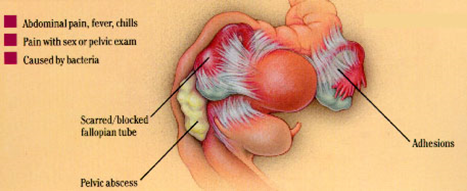
Salpingitis

Salpingitis is inflammation of the fallopian tubes. Almost all cases are caused by bacterial infection, including sexually transmitted diseases such as gonorrhoea and chlamydia. The inflammation prompts extra fluid secretion or even pus to collect inside the fallopian tube. Infection of one tube normally leads to infection of the other, since the bacteria migrates via the nearby lymph vessels.
Salpingitis is one of the most common causes of female infertility. Without prompt treatment, the infection may permanently damage the fallopian tube so that the eggs released each menstrual cycle can't meet up with sperm. Treatment options include antibiotics. Salpingitis is sometimes called pelvic inflammatory disease (PID). This umbrella term includes other infections of the female reproductive system, including the uterus and ovaries.
Symptoms
In milder cases, salpingitis may have no symptoms. This means the fallopian tubes may become damaged without the woman even realising she has an infection. The symptoms of salpingitis may include:
- Abnormal vaginal discharge, such as unusual colour or smell
- Spotting between periods
- Dysmenorrhoea (painful periods)
- Pain during ovulation
- Uncomfortable or painful sexual intercourse
- Fever
- Abdominal pain on both sides
- Lower back pain
- Frequent urination
- Nausea and vomiting
- The symptoms usually appear after the menstrual period.
Acute and chronic salpingitis
Salpingitis is usually categorised as either acute or chronic. In acute salpingitis, the fallopian tubes become red and swollen, and secrete extra fluid so that the inner walls of the tubes often stick together. The tubes may also stick to nearby structures such as the intestines. Sometimes, a fallopian tube may fill and bloat with pus. In rare cases, the tube ruptures and causes a dangerous infection of the abdominal cavity (peritonitis). Chronic salpingitis usually follows an acute attack. The infection is milder, longer lasting and may not produce many noticeable symptoms.
Most cases are caused by bacteria
In nine out of 10 cases of salpingitis, bacteria are the cause. Some of the most common bacteria responsible for salpingitis include:
- Chlamydia
- Gonococcus (which causes gonorrhoea)
- Mycoplasma
- Staphylococcus
- Streptococcus.
Access to the reproductive system
The bacteria must gain access to the woman's reproductive system for infection to take place. The bacteria can be introduced in a number of ways, including:
- Sexual intercourse
- Insertion of an IUD (intra-uterine device)
- Miscarriage
- Abortion
- Childbirth
- Appendicitis.
Lifestyle risk factors
Lifestyle factors that significantly increase a woman's risk of contracting salpingitis include:
- Engaging in sexual intercourse without a condom
- Prior infection with a sexually transmitted disease.
Complications of salpingitis
Without treatment, salpingitis can cause a range of complications, including:
- FURTHER INFECTION - the infection may spread to nearby structures, such as the ovaries or uterus.
- INFECTION OF SEX PARTNERS - the woman's partner or partners may contract the bacteria and become infected too.
- TUBO-OVARIAN ABSCESS - about 15 per cent of women with salpingitis develop an abscess, which requires hospitalisation.
- ECTOPIC PREGNANCY - a blocked fallopian tube prevents the fertilised egg from entering the uterus. The embryo then starts growing inside the confined space of the fallopian tube. The risk of ectopic pregnancy for a woman with prior salpingitis or other form of pelvic inflammatory disease (PID) is around one in 20.
- INFERTILITY - the fallopian tube may become deformed or scarred to such an extent that the egg and sperm are unable to meet. After one bout of salpingitis or other PID, a woman's risk of infertility is about 15 per cent. This rises to 50 per cent after three bouts.
Diagnosis methods
Diagnosing salpingitis involves a number of tests, including:
- GENERAL EXAMINATION - to check for localised tenderness and enlarged lymph glands.
- PELVIC EXAMINATION - to check for tenderness and discharge.
- BLOOD TESTS - to check the white blood cell count and other factors that indicate infection.
- MUCUS SWAB - a smear is taken to be cultured and examined in a laboratory so that the type of bacteria can be identified.
- LAPAROSCOPY - in some cases, the fallopian tubes may need to be viewed by a slender instrument inserted through abdominal incisions.
Treatment options
Treatment depends on the severity of the condition, but may include:
- ANTIBIOTICS - to kill the infection, which is successful in around 85 per cent of cases.
- HOSPITALISATION - including intravenous administration of antibiotics.
- SURGERY- if the condition resists drug treatment.
Pelvic Inflammatory Disease – PID
Pelvic inflammatory disease (PID) occurs when an infection spreads from the vagina to the cervix, endometrium (lining of the uterus) and fallopian tubes. The infection is usually sexually transmitted. It can also occur after a ruptured (burst) appendix or a bowel infection.
Some surgical procedures, such as abortion or insertion of an intrauterine device (IUD), can lead to PID.
The infection usually occurs in three stages - the cervix is infected first, followed by the endometrium and then the fallopian tubes.
The silent epidemic
PID is often called the ‘silent epidemic’ because it is common among sexually active women but does not always cause symptoms. About 10,000 women in Australia are treated for PID in hospital each year. About 10 to 30 times that number are treated as outpatients. Women aged 20 to 29 have the highest reported incidence of PID.
Signs and symptoms that can occur
Signs and symptoms of PID that may occur include:
- Lower abdominal pain or tenderness
- Menstrual disturbances
- Burning pain when urinating (dysuria)
- A change in smell, colour or amount of vaginal discharge
- Deep pain during sexual intercourse
- Fever.
Female infertility can be a devastating consequence
Scarring and blockage of the fallopian tubes is the most frequent long term complication of PID. Infertility occurs because the fertilised egg cannot pass through the tube to the uterus:
- One episode of PID doubles the risk of tubal infertility.
- The risk of fallopian tube blockage rises to 75 per cent after three or more episodes of PID.
- The risk of ectopic pregnancy (where the foetus develops outside the uterus) after one episode of PID is increased seven fold.
Chlamydia and gonorrhoea are the most common causes of PID
Chlamydia is responsible for 50 per cent of PID cases while gonorrhoea is the cause in 25 per cent of cases. The risk of fallopian tube blockage is slightly higher for PID caused by gonorrhoea. Both are bacterial infections and are sexually transmitted diseases (STDs). Non-specific urethritis, the most common STD among men, is most often caused by chlamydia.
Diagnosing PID
Your doctor will test for possible causes like chlamydia and gonorrhoea. In some cases, laparoscopy is required to correctly diagnose PID. Laparoscopy involves inserting an endoscope (which is like a surgical video camera) into the abdomen to view the reproductive organs.
Without treatment, chronic pain may develop
Chronic pain and, sometimes, severe disability can occur if PID is not treated. This is usually due to extensive scarring. Treatment involves:
- ANTIBIOTICS that are active against a broad range of organisms - amoxycillin (a type of penicillin) and doxycycline are usually prescribed.
- TESTING and TREATING male partners and treating them, if necessary - symptoms may be mild or non-existent in men.
- AVOIDING GENITAL SEXUAL XONTACT until the treatment is complete and a negative test result is obtained.
- SURGERY to remove scar tissue.
Protecting yourself from PID
To help prevent the transmission of the bacteria that can cause PID:
- Use condoms during vaginal or anal intercourse.
- Use condoms if you have an intrauterine device (IUD) inserted.
Use of the oral contraceptive pill may help
Sexually active women who are on the pill appear to have only one-third the risk of PID compared to women not on the pill. However, this data was collected in the 1970s and it is not known if the lower-dose pills more commonly used now have the same protective effect, although it is likely that they do.
Friday, November 27, 2009
What is trichomoniasis?
Trichomoniasis, sometimes referred to as "trich", is a common cause of vaginitis. It is caused by the single-celled protozoan parasite Trichomonas vaginalis. Trichomoniasis is primarily an infection of the urogenital tract; the most common site of infection is the urethra and the vagina in women.
Trichomoniasis is a common sexually transmitted disease (STD) that affects both women and men, although symptoms are more common in women.
How common is trichomoniasis?
Trichomoniasis is the most common curable STD in young, sexually active women. An estimated 7.4 million new cases occur each year in women and men.
How do people get trichomoniasis?
Trichomoniasis is caused by the single-celled protozoan parasite, Trichomonas vaginalis. The vagina is the most common site of infection in women, and the urethra (urine canal) is the most common site of infection in men.
The parasite is sexually transmitted through penis-to-vagina intercourse or vulva-to-vulva (the genital area outside the vagina) contact with an infected partner. Women can acquire the disease from infected men or women, but men usually contract it only from infected women.
What are the signs and symptoms of trichomoniasis?
Most men with trichomoniasis do not have signs or symptoms; however, some men may temporarily have an irritation inside the penis, mild discharge, or slight burning after urination or ejaculation.
Some women have signs or symptoms of infection which include a frothy, yellow-green vaginal discharge with a strong odor. The infection also may cause discomfort during intercourse and urination, as well as irritation and itching of the female genital area. In rare cases, lower abdominal pain can occur. Symptoms usually appear in women within 5 to 28 days of exposure.
What are the complications of trichomoniasis?
The genital inflammation caused by trichomoniasis can increase a woman’s susceptibility to HIV infection if she is exposed to the virus. Having trichomoniasis may increase the chance that an HIV-infected woman passes HIV to her sex partner(s).
How does trichomoniasis affect a pregnant woman and her baby?
Pregnant women with trichomoniasis may have babies who are born early or with low birth weight (low birth weight is less than 5.5 pounds)
How is trichomoniasis diagnosed?
For both men and women, a health care provider must perform a physical examination and laboratory test to diagnose trichomoniasis. The parasite is harder to detect in men than in women. In women, a pelvic examination can reveal small red ulcerations (sores) on the vaginal wall or cervix.
What is the treatment for trichomoniasis?
Trichomoniasis can usually be cured with prescription drugs, either metronidazole or tinidazole, given by mouth in a single dose. The symptoms of trichomoniasis in infected men may disappear within a few weeks without treatment. However, an infected man, even a man who has never had symptoms or whose symptoms have stopped, can continue to infect or re-infect a female partner until he has been treated. Therefore, both partners should be treated at the same time to eliminate the parasite. Persons being treated for trichomoniasis should avoid sex until they and their sex partners complete treatment and have no symptoms. Metronidazole can be used by pregnant women.
Having trichomoniasis once does not protect a person from getting it again. Following successful treatment, people can still be susceptible to re-infection.
How can trichomoniasis be prevented?
The surest way to avoid transmission of sexually transmitted diseases is to abstain from sexual contact, or to be in a long-term mutually monogamous relationship with a partner who has been tested and is known to be uninfected.
Latex male condoms, when used consistently and correctly, can reduce the risk of transmission of trichomoniasis.
Any genital symptom such as discharge or burning during urination or an unusual sore or rash should be a signal to stop having sex and to consult a health care provider immediately.
A person diagnosed with trichomoniasis (or any other STD) should receive treatment and should notify all recent sex partners so that they can see a health care provider and be treated. This reduces the risk that the sex partners will develop complications from trichomoniasis and reduces the risk that the person with trichomoniasis will become re-infected.
Sex should be stopped until the person with trichomoniasis and all of his or her recent partners complete treatment for trichomoniasis and have no symptoms.
Visitor
Labels
- Carcinoma (2)
- Dysmenorrhoea (4)
- Endometriosis (4)
- Female Genital Infection (3)
- Fluor Albus (4)
- General (3)
- Genital Prolapse (4)
- Gynecology (8)
- Infectious Disease in Pregnancy (13)
- Infertility (10)
- Menopause (3)
- Menstrual Disorder (10)
- Myoma Uteri (3)
- Obstetrics (13)
- Pelvic Floor (4)
- Pelvic Inflamatory Disease (3)
- Physiology of Human Reproductive System (4)
- Pregnancy (2)
- Sexually Transmitted Disease (6)
- Uterine Bleeding (4)
Followers
Facebook Badge
Copyright © 2009 Complicated Girl. All Rights Reserved.