Information Site About Reproductive System
About Me
Blog Archive
-
▼
2009
(58)
-
▼
December
(17)
- Syphilis During Pregnancy
- STDs and Pregnancy - Fact Sheet
- URINARY TRACT INFECTIONS in PREGNANCY
- GROUP B STREPTOCOCCUS INFECTION and PREGNANCY
- SWINE FLU and PREGNANCY
- GENITAL HERPES IN PREGNANCY
- LISTERIA and PREGNANCY
- REPIRATORY INFECTIONS DURING PREGNANCY
- HEPATITIS IN PREGNANCY
- CYTOMEGALOVIRUS
- CHLAMYDIA
- RUBELLA
- TOXOPLASMOSIS
- RECTOCELE
- CYSTOCELE
- PROLAPSE OF THE UTERUS
- PELVIC FLOOR
-
▼
December
(17)
Tuesday, December 1, 2009
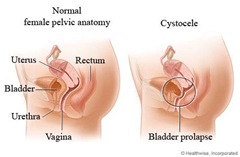
A cystocele is when the bladder bulges into the vagina.
Risk factors include vaginal childbirth, regularly straining on the toilet to pass bowel motions, obesity, smoking and chronic lung diseases with coughing.
Postmenopausal women are more susceptible to cystocele. This is because the sex hormone, oestrogen, helps to keep the muscles of the vagina and bladder – the pelvic floor muscles – in good tone. Once oestrogen levels drop, these muscles become thinner, weaker and less elastic. The vaginal skin stretches, which may allow the bladder to bulge into the vagina.
A cystocele can occur by itself or it may happen along with other abnormalities such as a rectocele (when the rectum protrudes into the vagina) or a uterine prolapse (when the uterus and cervix drop down to the vaginal entrance).
Treatment options include pelvic floor exercises, oestrogen therapy, inserting a pessary into the vagina to hold up the pelvic organs, and surgery. Other names for cystocele include prolapse of the bladder and ‘fallen’ bladder.
Symptoms
The symptoms of cystocele depend on individual factors, such as the severity of the condition, but can include:
- Stress incontinence – urine leaks when coughing, sneezing, laughing, standing up, running or walking
- Inability to completely empty the bladder after going to the toilet
- Recurring urinary tract infections (UTIs)
- Urination problems, such as straining to get urine flow started or an unusually slow flow of urine that tends to stop and start
- A sensation of fullness or pressure inside the vagina
- A bulging mass felt on the front wall of the vagina
- In severe cases, the vagina and the bladder protrude out of the vaginal entrance.
Grades of severity
A cystocele is graded on its degree of severity:
- GRADE 1 – the bladder protrudes a little way into the vagina.
- GRADE 2 – the bladder protrudes so far into the vagina that it is close to the vaginal opening.
- GRADE 3 – the bladder protrudes out of the vagina.
A range of causes
The vagina and bladder are held apart by tissue known as the pubocervical fascia. Thinning, weakening or tearing of the pubocervical fascia, and poor tone of the supporting muscles and ligaments, allow the bladder to drop against the vaginal wall. Some of the events that may cause or contribute to the development of a cystocele include:
- Vaginal childbirth
- Repeated heavy lifting
- Habitually straining to pass bowel motions
- The drop in oestrogen levels that occurs at menopause.
Diagnosis
Cystocele is diagnosed using a number of tests including:
- MEDICAL HISTORY – to check for possible risk factors.
- PHYSICAL EXAMINATION– cases of grade 2 or 3 cystocele can be easily diagnosed by vaginal examination.
- VOIDING CYSTOURETHROGRAM – a rarely used special x-ray that is taken while the patient is urinating. This test reveals whether the flow of urine is affected by the cystocele and if there is significant urine left in the bladder after passing urine (residual urine).
- OTHER TESTS– such as a bladder or pelvic ultrasound, a urodynamics investigation or x-rays to exclude other possible causes of urinary problems.
Treatment
Treatment for cystocele depends on the severity of the condition, but can include:
- MILD CASES – when there are no symptoms, treatment may be unnecessary. Regular monitoring is needed to make sure the cystocele doesn’t worsen. The doctor may advise a few lifestyle changes to prevent the condition getting worse, including doing pelvic floor exercises to strengthen the pelvic floor muscles.
- MODERATE CASES – a pessary is a small ring-like device that’s inserted high in the vagina. This is used temporarily in younger women and helps to keep the bladder in place. Health risks of long-term pessary use include infection and ulceration. This is more likely to be used in elderly women who are considered unfit for surgery due to chronic medical conditions.
- SEVERE CASES where symptoms impair quality of life. There are many different surgical techniques now available.
Pelvic floor physiotherapy
Pelvic floor exercises help to increase the strength of the pelvic floor muscles. They may reduce the symptoms felt as the result of a moderate to large cystocele. These exercises may also reduce symptoms of stress incontinence, which is often associated with a cystocele. It is important to learn to do the exercises correctly to gain the most benefit. There are specially trained physiotherapists or other health professionals available to help teach the correct techniques.
Surgery
Surgery for cystocele repair is usually done under general anaesthesia but also may be done under spinal or epidural anaesthesia. There are now many different types of surgery available depending on the symptoms a woman has. Traditionally, the vaginal wall is cut, the bladder is pushed away from the vagina and the excess vaginal tissue is removed. The bladder is supported by sutures into the pubocervical fascia and then the vagina is closed.
Mesh, graft or tape may be used to hold the bladder and urethra in place. Some procedures may be performed laparoscopically. Other procedures performed during the operation depend on individual factors: for example, a vagina overstretched by childbirth may be tightened.
A urinary catheter may be worn for between one and six days following surgery depending on the type of operation performed. Full recovery takes around four to six weeks.
Self-care suggestions
Your doctor may advise that you make a few lifestyle changes to prevent the cystocele from worsening or recurring after surgery. These suggestions may include:
- Don’t lift heavy objects.
- Increase the amount of fibre in your diet to prevent constipation and straining.
- Drink between six and eight glasses of water each day. Not drinking enough water makes stools hard, dry and difficult to pass.
- Exercise daily to help keep you regular.
- Use stool softeners, which may help in the short term.
- Avoid straining on the toilet for either bowels or bladder; use the hissing or sighing technique.
- Perform pelvic floor exercises daily to strengthen the muscles supporting the pelvic organs. You may need instruction from your doctor or other health care professional, such as a pelvic floor rehabilitation physiotherapist.
- Always squeeze up your pelvic floor muscles before you lift, cough, laugh or sneeze.
- If you are postmenopausal, your doctor may recommend hormone therapy, usually in the form of local oestrogen preparations such as a cream or a vaginal tablet, to help tone the muscles supporting the vagina and bladder.
- Seek medical advice for any condition that causes coughing and sneezing such as asthma, chest infections and hay fever.
- Keep yourself within a healthy weight range.
- Avoid sit-ups. Learn how to strengthen your deep abdominal muscles, but avoid straining.
Point to remember
- A cystocele is when the bladder bulges out into an overstretched vagina.
- Risk factors include vaginal childbirth and regularly straining on the toilet to pass bowel motions.
- Severe cases of cystocele need surgical repair.
Labels: Genital Prolapse, Gynecology, Pelvic Floor
Visitor
Labels
- Carcinoma (2)
- Dysmenorrhoea (4)
- Endometriosis (4)
- Female Genital Infection (3)
- Fluor Albus (4)
- General (3)
- Genital Prolapse (4)
- Gynecology (8)
- Infectious Disease in Pregnancy (13)
- Infertility (10)
- Menopause (3)
- Menstrual Disorder (10)
- Myoma Uteri (3)
- Obstetrics (13)
- Pelvic Floor (4)
- Pelvic Inflamatory Disease (3)
- Physiology of Human Reproductive System (4)
- Pregnancy (2)
- Sexually Transmitted Disease (6)
- Uterine Bleeding (4)
Followers
Facebook Badge
Copyright © 2009 Complicated Girl. All Rights Reserved.





0 comments:
Post a Comment