Information Site About Reproductive System
About Me
Blog Archive
-
▼
2009
(58)
-
▼
December
(17)
- Syphilis During Pregnancy
- STDs and Pregnancy - Fact Sheet
- URINARY TRACT INFECTIONS in PREGNANCY
- GROUP B STREPTOCOCCUS INFECTION and PREGNANCY
- SWINE FLU and PREGNANCY
- GENITAL HERPES IN PREGNANCY
- LISTERIA and PREGNANCY
- REPIRATORY INFECTIONS DURING PREGNANCY
- HEPATITIS IN PREGNANCY
- CYTOMEGALOVIRUS
- CHLAMYDIA
- RUBELLA
- TOXOPLASMOSIS
- RECTOCELE
- CYSTOCELE
- PROLAPSE OF THE UTERUS
- PELVIC FLOOR
-
▼
December
(17)
Friday, November 27, 2009
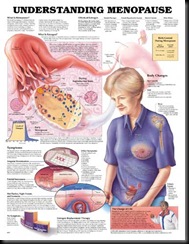
Menopause occurs when a woman stops ovulating and her monthly period (menstruation) ceases. It is a natural event that marks the end of the reproductive years.
The production of sex hormones, in particular oestrogen, falls significantly around menopause. Testosterone levels in women slowly decline from about 30 years of age. A woman in her forties has, on average, half the testosterone circulating in her bloodstream as a woman in her twenties.
The reduction of these hormones may directly affect libido or sex drive and sexual function for some women. It may also cause physical and psychological changes that will affect sexual function.
Other important issues that may influence the menopausal woman’s sexual desire and activity include contraception, physical changes (such as a dry, painful vagina), body image, relationship issues, illness and external stresses.
Contraception
Pregnancy is possible, though rare, before and even after your last period. It is generally advised that menopausal women should use contraception until at least one year after their natural periods have ceased. This is because a pregnancy late in a woman’s reproductive life increases the risk of birth defects for the child and health problems for the mother.
Hormone replacement therapy (HRT) is not a form of contraception. HRT is prescribed by a doctor to help manage the symptoms of a woman’s menopause. However, HRT does not contain sufficient hormones to suppress ovulation, so pregnancy can still occur.
There are many different options for contraception, which need to be discussed with your doctor.
Women who are sexually active should also continue to use condoms to protect against sexually transmissible infections (STIs). When using a condom, choose a water-based lubricant to avoid condom breakage.
Physical changes
Both during and after menopause, a woman may notice certain physical changes that affect her sexuality in positive and negative ways. These changes may include:
- Vaginal changes –as oestrogen levels fall, the walls of the vagina become thinner and drier. This loss of lubrication can make having sex uncomfortable.
- Slowed sexual response – getting aroused and reaching orgasm may take longer and be less intense.
- Infections – the post-menopausal vagina and bladder are more susceptible to bacterial infections.
- Menopause symptoms – such as hot flushes, night sweats, insomnia and unusual skin sensations like prickling or itching.
- Touch avoidance – some women can’t bear to be touched. Their skin feels more sensitive and they may recoil from closeness, particularly sexual intimacy. The physical discomfort of menopause symptoms may reduce a woman’s interest in sex or make her tired. Even the close proximity of her partner may be distressing because of the combined body heat.
- Absent periods – a woman who was troubled by heavy or painful periods may feel relieved and positive about her change of life. This can lead to a renewed interest in sex.
- No fear of pregnancy – many women who were trying to avoid pregnancy during their reproductive years may find the menopause begins a time of renewed sexual interest. Without the fear of possible pregnancy, sex becomes relaxed, fun and more frequent.
Body image
Some of the issues that may contribute to a menopausal woman’s body image include:
- Social attitudes – Western culture tends to value youth, thinness and beauty, while older women are rarely portrayed as sexual or desirable. These ingrained social attitudes may prompt some women who are approaching the menopause to feel less attractive. Other women may erroneously believe that sex is only for the young, and this attitude can cause sexual interest and activity to wane.
- Weight gain – an increase in body fat, especially around the abdomen, can occur during menopause because of hormonal changes. The age-related decrease in muscle tissue and the associated slowing of the metabolism also contribute.
- Changes to body hair – some women experience abnormal hair growth after menopause, particularly on the face. Others may experience thinning of scalp and pubic hair.
Other issues
Other issues that may impact on a woman’s sexuality during and after menopause include:
- Ill-health – since disorders such as cardiovascular disease and osteoporosis are more prevalent in older women.
- Some medications – such as some antidepressants or antihypertensives, which may affect sexual function and libido.
- Ill-health or sexual difficulties of a partner – such as erectile problems.
- Loss of a partner – through death, divorce or separation.
- Depression
- Children leaving or staying at home – children leaving home allows more sexual freedom for the older couple; children staying at home may restrict independence; the ‘revolving door’, with children coming and going, can also have an impact.
Enhance your sex life
Suggestions to maintain or improve your sex life after the menopause include:
- Talk openly with your partner about sex and the impacts – both positive and negative – of menopause.
- Physical changes may slow your reaction times. Plan for slow, lingering sessions of lovemaking.
- Try widening your sexual horizons and include sexual activities that don’t involve vaginal penetration such as oral sex, sexual aids and mutual masturbation.
- Regular masturbation helps to improve blood flow and muscle tone.
- Wash your vulva with warm water and sorbolene rather than soap, which can further dry and irritate the tissues.
- If vaginal dryness persists, consider using water-based vaginal lubricants, available from pharmacists and supermarkets.
- Vaginal preparations of oestrogen creams, tablets and pessaries or hormone replacement therapy can help manage vaginal dryness. Consult with your doctor.
- Exercise regularly and eat a healthy diet to maintain an appropriate weight for your height.
- Oestrogen plus testosterone therapy may affect sexuality positively.
- Seek advice from a professional if you need help with any sexual issues.
- Relationship or sexual counselling may help resolve issues with partners.
Labels: Menopause
Many women, although not all, experience uncomfortable symptoms during and after menopause, including hot flushes, night sweats and vaginal dryness. These symptoms, and the associated physical changes, can be managed in various ways including education and lifestyle changes like diet and exercise.
Hormone replacement therapy (HRT) is also available if required. This is also known as hormone therapy (HT). While HRT reduces the risk of some debilitating diseases, it also increases the risk of others.
Menopause occurs when a woman stops ovulating, the ovaries no longer produce oestrogen (one of the female sex hormones) and her monthly period (menstruation) ceases. It is a natural event that marks the end of the reproductive years, just as the first menstrual period during puberty marked the start.
Menopause symptoms can be reduced by HRT
The following menopause-related symptoms may be reduced by HRT:
- Hot flushes
- Night sweats
- Vaginal dryness
- Thinning of vaginal walls
- Vaginal and bladder infections
- Mild urinary incontinence
- Insomnia
- Cognitive changes, such as memory loss
- Reduced sex drive
- Mood disturbance
- Abnormal sensations, such as ‘prickling’ or ‘crawling’ under the skin
- Palpitations
- Hair loss or abnormal growth
- Dry and itching eyes
- Tooth loss
- Gingivitis (gum problems).
Side effects of HRT
HRT needs to be individually tailored. Some women experience side effects during the early stages of treatment, which may include:
- Breakthrough bleeding
- Breast tenderness
- Bloating – around one in 10,000 women aged 50 experience bloating and this increases with age
- Blood clots – the risk increases with age. Younger women on oral HRT face a one in 5,000 to one in 10,000 risk of blood clots. Older women, aged 50 to 60 years, face a one in 500 to one in 1,000 risk of blood clots when on oral HRT.
HRT does not cause weight gain
An increase in body fat, especially around the abdomen, can occur during menopause because of our own hormonal changes, although exactly why this happens is not clear. The age-related decrease in muscle tissue and the slowing down of the metabolism can also contribute to weight gain.
Various studies prove that weight gain is not linked to HRT. If a woman is prone to weight gain during her middle years, she will do so regardless of whether or not she uses HRT. Some women may experience symptoms at the start of treatment, including bloating and breast fullness, which may be misinterpreted as weight gain. These symptoms usually disappear once the therapy doses are modified to suit the individual.
Contraception is still needed
HRT is not a form of contraception. The treatment does not contain sufficient hormones to suppress ovulation, so pregnancy is still possible in women who are ovulating occasionally in the perimenopause. It is generally advised that menopausal women should continue to use contraception until their natural periods have ceased for at least one year.
Long-term use of HRT to prevent disease
HRT reduces the risk of various chronic conditions that can affect postmenopausal woman, including:
- Osteoporosis – thinning of the bones to the point where they break easily. HRT prevents further bone loss, which preserves bone integrity and reduces the risk of fractures, but is not recommended as a first-line treatment.
- Bowel cancer – the risk of colorectal cancers is slightly reduced with HRT.
HRT- related health risks
While HRT reduces the risk of some debilitating diseases, it also increases the risk of others. These small risks must be balanced against the benefits for the individual. Three areas of concern are:
- Breast cancer – current research suggests that women over 50 years of age, who use oestrogen and progestogen replacement for less than five years, have little or no increased risk of breast cancer. Women who use HRT with progestogen for more than five years appear to have a slightly increased risk. Women on oestrogen alone appear to have no increased risk up to 15 years of usage. There is no evidence to suggest that a woman with a family history of breast cancer will have an added increased risk of developing the disease if she uses HRT. The risk with combined oestrogen and progestogen is greater than with oestrogen alone or with newer HRT agents, including Tibolone, but research in this area is ongoing.
- Cardiovascular disease – current research suggests that women over 60 have a small increased risk of developing both heart disease and strokes on combined oral HRT. Although this risk is small (7 heart attacks and 8 strokes per 10,000 treatment years – that is, 1,000 women treated for 10 years), it needs to be considered when starting HRT, as the risk occurs early in treatment and persists with time. Oestrogen used on its own increases the risk of stroke (12 per 1,000 women per year). Women who commence HRT around the time of menopause may not have the same increased risk as women aged 60 or more. The risk with other forms of hormone therapy such as Tibolone is unknown. The results of ongoing research are awaited with interest.
- Thrombosis – these are blood clots that form inside veins. Some women on HRT are more likely to get thrombosis than women who are not on HRT. This risk seems to be highest in the first one to two years of therapy and in women who have a high risk of blood clots anyway. This especially applies to women who have a genetic predisposition to developing thrombosis. More research is needed to clarify if oestrogen applied through the skin as patches, implants or gels has the same effect. Limited research to date would suggest the increased risk of clots is mainly related to oestrogen and progestogen in tablet form.
- Endometrial cancer – this is cancer of the lining of the uterus. Long-term use (for 10 years or more) of oestrogen alone increases the risk of this cancer, but this risk is neutralised with the addition of progestogen to the treatment.
Long-term use is not recommended
It is currently believed that, overall, the risks of long-term HRT use outweigh the benefits. HRT should not be recommended for disease prevention. However, the jury is still out on the use of oestrogen alone, other HRT preparations (including Tibolone) and other forms of HRT (including patches). We await the results of further trials before recommendations in these areas can be made.
However, in women with long-term severe symptoms, HRT may be the only effective therapy. Seek specialist advice from a menopause clinic or specialist physician. Regular check-ups are recommended.
HRT and prior history of breast cancer
To date, there is conflicting specific evidence that HRT will increase the risk of breast cancer recurring in a woman with a prior history of the disease. However, oestrogen and progestins may stimulate some types of cells in the breast and increase the risk of breast cancer in women without a history of breast cancer. It is advisable for woman with a prior history of breast cancer to avoid HRT.
Phytoestrogens and prior history of breast cancer
There is no evidence that phytoestrogens increase the risk of breast cancer recurring but, under certain circumstances, some breast cells may be stimulated. Other forms of management for menopausal symptoms may be advised, such as oestrogen vaginal creams or low doses of antidepressants, which may reduce hot flushes. Be advised by your doctor.
Alternative therapies
Alternative therapies for the management of menopausal symptoms remain controversial. Many of these therapies have not been subjected to clinical trials, so their effectiveness is based on the experiences reported by some women. To date, no alternative therapy has been clinically proven to reduce a menopausal woman’s risk of osteoporosis, and preliminary studies would suggest there is no benefit for the bones. Some of the more popular alternative therapies include:
- Soy products
- Phytoestrogens
- Herbal medicines.
Labels: Menopause
Wednesday, November 11, 2009
Definition
Menopause is the permanent end of menstruation and fertility, defined as occurring 12 months after your last menstrual period.
Menopause is a natural biological process, not a medical illness. Even so, the physical and emotional symptoms of menopause can disrupt your sleep, sap your energy and — at least indirectly — trigger feelings of sadness and loss.
Hormonal changes cause the physical symptoms of menopause, but mistaken beliefs about the menopausal transition are partly to blame for the emotional ones. First, menopause doesn't mean the end is near — you've still got as much as half your life to go. Second, menopause will not snuff out your femininity and sexuality. In fact, you may be one of the many women who find it liberating to stop worrying about pregnancy and periods.
Most important, even though menopause is not an illness, you shouldn't hesitate to get treatment if you're having severe symptoms. Many treatments are available, from lifestyle adjustments to hormone therapy.
Symptoms
Technically, you don't actually "hit" menopause until it's been one year since your final menstrual period. Menopause, that happens about age 51, on average.
The signs and symptoms of menopause, however, often appear long before the one-year of your final period. They include:
- Irregular periods
- Decreased fertility
- Vaginal dryness
- Hot flashes
- Sleep disturbances
- Mood swings
- Increased abdominal fat
- Thinning hair
- Loss of breast fullness
When to see a doctor
It's important to see your doctor during the years leading up to menopause (perimenopause) and the years after menopause (postmenopause) for preventive health care as well as care of medical conditions that may occur with aging.
If you've skipped a period but aren't sure you've started menopause, you may want to see your doctor to determine whether you're pregnant. He or she may take a medical history, do a pelvic examination and, if appropriate, order a pregnancy test.
Always seek medical advice if you have bleeding from your vagina after menopause.
Causes
Causes of menopause include:
- Natural decline of reproductive hormones. As you approach your late 30s, your ovaries start making less estrogen and progesterone, the hormones that regulate menstruation. During this time, fewer potential eggs are ripening in your ovaries each month, and ovulation is less predictable. Also, the post-ovulation surge in progesterone — the hormone that prepares your body for pregnancy — becomes less dramatic. Your fertility declines, partially due to these hormonal effects.
These changes become more pronounced in your 40s. Your menstrual periods may become longer or shorter, heavier or lighter, and more or less frequent, until eventually, your ovaries stop producing eggs, and you have no more periods. It's possible, but very unusual, to menstruate every month right up to your last period. More likely, you'll experience some irregularity in your periods.
- Hysterectomy. A hysterectomy that removes your uterus, but not your ovaries, usually doesn't cause menopause. Although you no longer have periods, your ovaries still release eggs and produce estrogen and progesterone. But an operation that removes both your uterus and your ovaries (total hysterectomy and bilateral oophorectomy) does cause menopause, without any transitional phase. Your periods stop immediately, and you're likely to have hot flashes and other menopausal signs and symptoms.
- Chemotherapy and radiation therapy. These cancer therapies can induce menopause, causing symptoms such as hot flashes during the course of treatment or within three to six months.
- Primary ovarian insufficiency. Approximately 1 percent of women experience menopause before age 40. Menopause may result from primary ovarian insufficiency — when your ovaries fail to produce normal levels of reproductive hormones — stemming from genetic factors or autoimmune disease, but often no cause for primary ovarian insufficiency can be found.
Stages of menopause
Because the menopausal transition occurs over months and years, menopause is commonly divided into these stages:
- Perimenopause. This is the time you begin experiencing menopausal signs and symptoms, even though you still menstruate. Your hormone levels rise and fall unevenly, and you may have hot flashes and other symptoms. Perimenopause may last four to five years or longer. During this time, it's still possible to get pregnant, but it's quite unlikely.
- Postmenopause. Once 12 months have passed since your last period, you've reached menopause. Your ovaries produce much less estrogen and no progesterone, and they don't release eggs. The years that follow are called postmenopause.
Complications
Several chronic medical conditions can develop after menopause:
- Cardiovascular disease. When your estrogen levels decline, your risk of cardiovascular disease increases. Heart disease is the leading cause of death in women as well as in men. Yet you can do a great deal to reduce your risk of heart disease. These risk-reduction steps include stopping smoking, reducing high blood pressure, getting regular aerobic exercise, and eating a diet low in saturated fats and plentiful in whole grains, fruits and vegetables.
- Osteoporosis. During the first few years after menopause, you may lose bone density at a rapid rate, increasing your risk of osteoporosis. Osteoporosis causes bones to become brittle and weak, leading to an increased risk of fractures. Postmenopausal women are especially susceptible to fractures of the hip, wrist and spine. That's why it's important during this time to get adequate calcium and vitamin D — about 1,200 to 1,500 milligrams of calcium and 800 international units of vitamin D daily. It's also important to exercise regularly. Strength training and weight-bearing activities, such as walking and jogging, are especially beneficial in keeping your bones strong.
- Urinary incontinence. As the tissues of your vagina and urethra lose their elasticity, you may experience a frequent, sudden, strong urge to urinate, followed by an involuntary loss of urine (urge incontinence), or the loss of urine with coughing, laughing or lifting (stress incontinence).
- Weight gain. Many women gain weight during the menopausal transition. You may need to eat less — perhaps as many as 200 to 400 fewer calories a day — and exercise more, just to maintain your current weight.
Preparing for your appointment
Your first appointment will likely be with either your primary care provider or a gynecologist.
Because appointments can be brief, and it can be difficult to remember everything you want to discuss, it's a good idea to prepare in advance of your appointment.
What you can do
- Keep track of symptoms you're experiencing. For instance, write down how many hot flashes you experience in a day or week and note how severe they are.
- Make a list of any medications and vitamin supplements you take. Write down doses and how often you take them.
- Have a family member or close friend accompany you, if possible. You may be given a lot of information at your visit, and it can be difficult to remember everything.
- Take a notebook or notepad with you. Use it to write down important information during your visit.
- Prepare a list of questions to ask your doctor. List your most important questions first, in case time runs out.
Some basic questions to ask include:
- What kind of tests might I need?
- What treatments are available to minimize my symptoms?
- Is there anything I can do to relieve my symptoms?
- What steps can I take to maintain my health?
- Do you have any printed material or brochures I can take with me? What Web sites do you recommend?
Make sure that you understand everything that your doctor tells you. Don't hesitate to ask your doctor to repeat information or to ask follow-up questions for clarification.
What to expect from your doctor
Some potential questions your doctor might ask include:
- Are you still having periods?
- When was your last period?
- How often do you experience bothersome symptoms?
- How uncomfortable do your symptoms make you?
- Does anything seem to improve your symptoms?
- Does anything make your symptoms worse?
Tests and diagnosis
The signs and symptoms of menopause are enough to tell most women they have begun going through the menopausal transition. If you have concerns about irregular periods or hot flashes, talk with your doctor. In some cases further evaluation may be recommended.
Under certain circumstances, your doctor may check your level of follicle-stimulating hormone (FSH) and estrogen (estradiol) with a blood test. As menopause occurs, FSH levels increase and estradiol levels decrease. Your doctor may also recommend a blood test to determine your level of thyroid-stimulating hormone (TSH ) , because hypothyroidism can cause symptoms similar to those of menopause.
Treatments and drugs
Menopause itself requires no medical treatment. Instead, treatments focus on relieving your signs and symptoms and on preventing or lessening chronic conditions that may occur with aging. Treatments include:
- Hormone therapy. Estrogen therapy remains, by far, the most effective treatment option for relieving menopausal hot flashes. Depending on your personal and family medical history, your doctor may recommend estrogen in the lowest dose needed to provide symptom relief for you.
- Low-dose antidepressants. Venlafaxine (Effexor), an antidepressant related to the class of drugs called selective serotonin reuptake inhibitors (SSRIs), has been shown to decrease menopausal hot flashes. Other SSRIs can be helpful, including fluoxetine (Prozac, Sarafem), paroxetine (Paxil, others), citalopram (Celexa) and sertraline (Zoloft).
- Gabapentin (Neurontin). This drug is approved to treat seizures, but it also has been shown to significantly reduce hot flashes.
- Clonidine (Catapres, others). Clonidine, a pill or patch typically used to treat high blood pressure, may significantly reduce the frequency of hot flashes, but unpleasant side effects are common.
- Bisphosphonates. Doctors may recommend these nonhormonal medications, which include alendronate (Fosamax), risedronate (Actonel) and ibandronate (Boniva), to prevent or treat osteoporosis. These medications effectively reduce both bone loss and your risk of fractures and have replaced estrogen as the main treatment for osteoporosis in women.
- Selective estrogen receptor modulators (SERMs). SERMs are a group of drugs that includes raloxifene (Evista). Raloxifene mimics estrogen's beneficial effects on bone density in postmenopausal women, without some of the risks associated with estrogen.
- Vaginal estrogen. To relieve vaginal dryness, estrogen can be administered locally using a vaginal tablet, ring or cream. This treatment releases just a small amount of estrogen, which is absorbed by the vaginal tissue. It can help relieve vaginal dryness, discomfort with intercourse and some urinary symptoms.
Before deciding on any form of treatment, talk with your doctor about your options and the risks and benefits involved with each.
Lifestyle and home remedies
Fortunately, many of the signs and symptoms associated with menopause are temporary. Take these steps to help reduce or prevent their effects:
- Cool hot flashes. Get regular exercise, dress in layers and try to pinpoint what triggers your hot flashes. For many women, triggers may include hot beverages, spicy foods, alcohol, hot weather and even a warm room.
- Decrease vaginal discomfort. Use over-the-counter water-based vaginal lubricants (Astroglide, K-Y) or moisturizers (Replens, Vagisil). Staying sexually active also helps.
- Optimize your sleep. Avoid caffeine and plan to exercise during the day, although not right before bedtime. Relaxation techniques, such as deep breathing, guided imagery and progressive muscle relaxation, can be very helpful. You can find a number of books and tapes on different relaxation exercises. If hot flashes disturb your sleep, you may need to find a way to manage them before you can get adequate rest.
- Strengthen your pelvic floor. Pelvic floor muscle exercises, called Kegel exercises, can improve some forms of urinary incontinence.
- Eat well. Eat a balanced diet that includes a variety of fruits, vegetables and whole grains and that limits saturated fats, oils and sugars. Aim for 1,200 to 1,500 milligrams of calcium and 800 international units of vitamin D a day. Ask your doctor about supplements to help you meet these requirements, if necessary.
- Don't smoke. Smoking increases your risk of heart disease, stroke, osteoporosis, cancer and a range of other health problems. It may also increase hot flashes and bring on earlier menopause. It's never too late to benefit from stopping smoking.
- Exercise regularly. Get at least 30 minutes of moderate-intensity physical activity on most days to protect against cardiovascular disease, diabetes, osteoporosis and other conditions associated with aging. More vigorous exercise for longer periods may provide further benefit and is particularly important if you're trying to lose weight. Exercise can also help reduce stress.
- Try yoga. Preliminary studies show that yoga — an exercise regimen that involves controlled breathing, posing and meditation — may be effective in decreasing the number of hot flashes in perimenopausal women. Yoga classes are often offered at health clubs or through community education programs. Sign up for a class to learn how to perform yoga postures and breathing correctly.
- Schedule regular checkups. Talk with your doctor about how often you should have mammograms, Pap tests, lipid level (cholesterol and triglyceride) testing and other screening tests.
Alternative medicine
Many approaches have been promoted as aids in managing the symptoms of menopause, but not all of them have scientific evidence to back up the claims. Below are some complementary and alternative treatments that have been or are being studied:
- Phytoestrogens. These estrogens occur naturally in certain foods. There are two main types of phytoestrogens — isoflavones and lignans. Isoflavones are found in soybeans, chickpeas and other legumes. Lignans occur in flaxseed, whole grains and some fruits and vegetables. Whether the estrogens in these foods can relieve hot flashes and other menopausal signs and symptoms remains to be seen. Most studies have found them ineffective. Isoflavones have some weak estrogen-like effects, so there's some concern about cancer risk. If you've had breast cancer, talk to your doctor before supplementing your diet with isoflavone pills.
- Vitamin E. This vitamin occasionally provides relief from mild hot flashes for some women. However, scientific studies haven't proved its overall benefit in relieving hot flashes, and taking more than 400 international units of vitamin E supplements daily may not be safe.
- Black cohosh. Black cohosh has been used widely in Europe for treating hot flashes and has been popular among women with menopausal symptoms in the United States. While its safety record has been good, there's no longer much reason to believe that it is effective for menopausal symptom relief.
You may have heard of — or even tried — other dietary supplements, such as dong quai, licorice, chasteberry, evening primrose oil and wild yam (natural progesterone cream). Although some might swear by these remedies, scientific evidence of their safety and effectiveness is lacking.
Be sure to consult your doctor before taking any herbal treatments or dietary supplements for signs and symptoms of menopause. Herbal products can interfere or interact with other medications you may be taking.
Labels: Menopause
Visitor
Labels
- Carcinoma (2)
- Dysmenorrhoea (4)
- Endometriosis (4)
- Female Genital Infection (3)
- Fluor Albus (4)
- General (3)
- Genital Prolapse (4)
- Gynecology (8)
- Infectious Disease in Pregnancy (13)
- Infertility (10)
- Menopause (3)
- Menstrual Disorder (10)
- Myoma Uteri (3)
- Obstetrics (13)
- Pelvic Floor (4)
- Pelvic Inflamatory Disease (3)
- Physiology of Human Reproductive System (4)
- Pregnancy (2)
- Sexually Transmitted Disease (6)
- Uterine Bleeding (4)
Followers
Facebook Badge
Copyright © 2009 Complicated Girl. All Rights Reserved.