Information Site About Reproductive System
About Me
Blog Archive
-
▼
2009
(58)
-
▼
November
(20)
- HYSTERECTOMY – SURGICAL PROCEDURES
- HYSTERECTOMY
- MYOMECTOMY
- FIBROID
- GONORRHOEA INFECTION
- SALPINGITIS
- PELVIC INFLAMATORY DISEASE
- ENDOMETRIOSIS – Treatment Options
- ENDOMETRIOSIS – causes and risk factors
- ENDOMETRIOSIS
- ADENOMYOSIS
- HUMAN FERTILIZATION
- EARLY PREGNANCY SYMPTOMS
- MENOPAUSE and SEXUAL ISSUES
- CYTOLYTIC VAGINOSIS
- MENOPAUSE- hormone replacement therapy
- VULVOVAGINAL CANDIDIASIS
- TRICHOMONIASIS
- BACTERIAL VAGINOSIS
- MENOPAUSE
-
▼
November
(20)
Monday, November 30, 2009
| |
Hysterectomy is the surgical removal of a woman's uterus. It may also involve the removal of the fallopian tubes and ovaries. Once a hysterectomy is performed, a woman can no longer have children or menstrual periods.
Hysterectomy is used to treat a number of conditions, such as excessive menstrual bleeding and cancer. In Australia, around 30,000 women undergo this operation every year.
Conditions that may require hysterectomy
A hysterectomy may be performed to correct various gynaecological problems including:
- Heavy, irregular or abnormal menstrual bleeding
- Fibroids
- Endometriosis
- Uterine prolapse
- Cancer of the uterus, ovary or cervix
- Pelvic inflammatory disease.
Medical issues to consider
Apart from cancer, many of the gynaecological conditions assisted by hysterectomy may also be successfully treated using other methods. If, after discussion of all options with your doctor, you choose to have a hysterectomy, there are several things that your doctor should discuss with you before the operation. These include:
- Your medical history (as some pre-existing conditions may influence decisions on surgery and anaesthetics).
- The pros and cons of abdominal surgery versus vaginal surgery.
- Your support options after surgery.
- Your feelings about the surgery.
You will have a range of tests, including a complete blood count test to check for problems such as anaemia.
Operation procedure
You will have an intravenous drip inserted into a vein in your hand or arm, and will be given a general anaesthetic. The operation may be performed via a lower abdominal incision (cut) or through the vagina.
Abdominal hysterectomy
For an abdominal hysterectomy, a cut is usually made horizontally along your pubic hairline (and your pubic hair will be shaved around the incision). For most women, this results in a small scar. Some patients may need a vertical incision in the lower abdomen.
Vaginal hysterectomy
A vaginal hysterectomy is performed through an incision (cut) at the top of the vagina. This may or may not involve the use of a laparoscope. A laparoscope is a slender instrument used in 'keyhole' surgery. During a laparoscopic assisted vaginal hysterectomy, surgery is performed via three or four small incisions in the abdomen. It is completed through the vagina.
Vaginal hysterectomy is a preferred option for many women as it avoids the need for a long abdominal cut. An abdominal procedure is generally recommended when large fibroids or cancer is present.
Types of hysterectomy
There are four variations of hysterectomy, including:
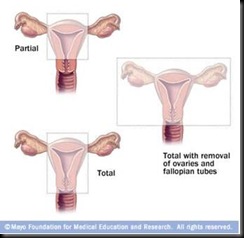
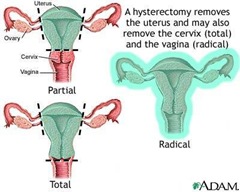
| |
- TOTAL HYSTERECTOMY - the entire uterus and cervix is removed, but the ovaries are retained.
- SUBTOTAL (partial)HYSTERECTOMY- the uterus is removed, but the cervix may be retained. While removal of the cervix is generally advised because it is a potential cancer site in the body, some women consider that it serves a purpose during penetrative sex. If the cervix is kept, regular Pap smears are necessary.
- HYSTERECTOMY and BILATERAL SALPHYNGOOPHARECTOMY - the uterus, fallopian tubes and ovaries are removed. This operation is performed if cancer of the ovaries or the uterus has been diagnosed. It may also be performed for severe infection or endometriosis.
- RADICAL HYSTERECTOMY - the most extensive version of the operation. It involves the removal of the uterus, fallopian tubes, ovaries, upper part of the vagina, and associated pelvic ligaments and lymph nodes. This may be performed if cancer of the cervix, ovaries or uterus is present.
Immediately after the operation
After the operation, you can expect:
- There will be some soreness around the operation site - your doctor will prescribe pain-killing medication for you.
- You may experience 'wind' pain for a few days.
- Depending on the procedure and your condition, the intravenous tube in your arm will be removed sometime during the first few days.
- The catheter (drainage tube) in your bladder is usually removed within 24 hours of surgery, unless the bladder was traumatised during the procedure.
- As soon as possible, you will be encouraged to get out of bed and go for short walks around the ward.
- Depending on the type of surgery, you can expect a hospital stay of between two and seven days.
- Recovery is generally faster after vaginal surgery than abdominal surgery.
Following surgery, it is important to start pelvic floor and abdominal exercises as soon as possible. These exercises strengthen the muscles in the pelvis and help maintain normal bladder function and vaginal muscle tone. Your doctor or physiotherapist will let you know how soon you can start these particular exercises.
Side effects and possible complications
Some of the side effects and possible complications of hysterectomy include:
- Nausea and vomiting.
- Infection.
- Internal haemorrhage.
- Build-up of blood beneath the stitches.
- Internal scar tissue.
- Allergic reaction to the anaesthetic.
- Blood clots.
- Vaginal vault prolapse.
- Feelings of grief and loss.
- Injury to the bowel, bladder or ureters (tubes that carry urine from the kidneys to the bladder) - this is rare.
- Fistula (abnormal hole between internal structures, such as the bowel and vagina). This is also rare.
Taking care of yourself at home
Be guided by your doctor, but general suggestions for the six week post-operative period include:
- REST - try to rest as much as possible for at least two weeks. You should avoid driving during this time.
- EXERCISE- continue with the exercises you were shown in hospital. After two weeks of rest, you should aim to go for a 10 minute walk each day, unless advised otherwise by your doctor.
- STANDING - avoid standing for more than a few minutes at a time in the early post-operative period. You can increase standing time as recovery progresses.
- LIFTING- avoid heavy lifting and stretching.
- CONSTIPATION - to avoid constipation, drink plenty of fluids and eat fresh fruits and vegetables. You may wish to take stool softeners for the first few days.
- MEDICATION - if you have been prescribed antibiotics, make sure you take the full course, even if you feel well.
- SEX - it is advised that you avoid penetrative sex until after the post-operative check (at about six weeks) to ensure the vagina is fully healed. If vaginal dryness is a problem, it may be helpful to use a water based lubricant.
Long term outlook
After hysterectomy, you will no longer need contraception or have menstrual periods. If your ovaries were removed, you will experience sudden menopause. You may want to discuss short term hormone replacement therapy (HRT) or other options with your doctor. Hysterectomy can be effective for gynaecological complaints like fibroids and endometriosis, but some conditions (such as cancer) may recur. You will need to have regular check-ups to make sure you are cancer free. You may need to have a regular vault smear. This test is similar to a Pap smear but it takes cells from the vaginal walls instead of the cervix.
Other forms of treatment
Many of the various gynaecological conditions cured by hysterectomy can often be successfully treated using other methods, including:
- FIBROID- options include surgery to remove the fibroids (myomectomy), drugs to temporarily block the action of sex hormones and shrink the growths, or else the fibroids can be frozen, cauterised or removed by laser (myolysis).
- HEAVY BLEEDING - options include taking the contraceptive pill to regulate the periods, other hormonal drug therapies, surgical removal of the endometrium, or the insertion of an intrauterine device (IUD) that releases small amounts of synthesised sex hormone into the uterus.
- UTERINE PROLAPSE- options include pelvic floor exercises, the insertion of a ring-shaped pessary into the vagina to prop up the uterus, or surgical repair.
- ENDOMETRIOSIS - options include hormonal drugs, surgical removal of the endometrium, or the insertion of an intrauterine device (IUD) that releases small amounts of synthesised sex hormone into the uterus.
- Hysterectomy is the surgical removal of the uterus.
- A hysterectomy may be performed to correct various gynaecological problems including abnormal menstrual bleeding, fibroids, endometriosis, and cancer of the uterus, ovary or cervix.
- The operation may be performed via an abdominal incision or through the vagina.
- Apart from cancer, many of the various gynaecological conditions cured by hysterectomy can often be successfully treated using other methods
Things to remember
Labels: Carcinoma, Gynecology, Myoma Uteri, Uterine Bleeding
Hysterectomy is the surgical removal of the womb (uterus), with or without the removal of the ovaries.
The uterus is a muscular organ of the female body, shaped like an inverted pear.
The lining of the uterus, the endometrium, thickens during ovulation in preparation for receiving a fertilised ovum. If the ovum is unfertilised, the lining comes away. This is known as menstruation. If the ovum is fertilised, the developing baby is nurtured inside the uterus throughout the nine months of pregnancy.
Once a hysterectomy is performed, a woman can no longer have children or menstrual periods. Hysterectomy is used to treat a number of conditions, such as excessive menstrual bleeding.
There are concerns that more hysterectomies are performed than are necessary.
Reasons for hysterectomy
The conditions that may be treated by hysterectomy include:
- FIBROIDS , which are non-malignant growths inside the muscular walls of the uterus.
- Heavy or irregular menstrual periods or MENORRHAGIA
- Severe period pain, or DYSMENORRHOEA.
- CANCER of the cervix, uterus or ovaries.
- ENDOMETRIOSIS , a condition characterised by the migration of cells from the lining the uterus to other areas of the body.
- PROLAPSE, which means the uterus falls into the vagina because of loose ligaments or damage to the pelvic floor muscles.
- PELVIC INFLAMATORY DISEASE , caused by bacterial infection.
Degrees of hysterectomy
There are three basic types of hysterectomy:
- TOTAL HYSTERECTOMY - removal of the uterus and cervix. The ovaries and tubes remain.
- SUBTOTAL HYSTERECTOMY - removal of the body of the uterus. The cervix, ovaries and the tubes remain.
- TOTAL HYSTERECTOMYY and BILATERAL SALPHYNGO OOPHORECTOMY - removal of the uterus, cervix, ovaries and tubes.
Different surgical procedures
The type of procedure used influences the length of hospital stay and recovery time. Hysterectomy procedures include:
- VAGINAL - the uterus is removed through an incision in the top-end of the vagina. There are no cuts to the abdomen.
- VAGINAL and LAPAROSCOPY - an instrument called a laparoscope is inserted through small abdominal incisions to assist in the vaginal removal of the uterus. During laparoscopic-assisted vaginal hysterectomy, surgery is performed through three to four small incisions in the abdomen and completed through the vagina.
- ABDOMINAL - the uterus is removed through a lower abdominal incision. With a total abdominal hysterectomy, surgery is performed through a long abdominal cut similar to that which is conducted for a caesarian section.
Possible complications
Possible complications of hysterectomy include:
- Difficulties with urination
- Decreased sexual desire
- Constant pelvic pain
- Psychological distress
- Complications of any operation or anaesthetic.
Women of childbearing age
Once a hysterectomy of any kind is performed, pregnancy is no longer possible.
If the ovaries of a premenopausal woman are removed, then ovulation will also cease. This means there will be a drop in production of the sex hormones oestrogen and progesterone, which can cause vaginal dryness, hot flushes, sweating and other associated symptoms of natural menopause.
Women who undergo bilateral oophorectomy, or removal of both ovaries, are usually treated with hormone replacement therapy (HRT) - also known as hormone therapy (HT) - to maintain their hormone levels.
The other roles of the uterus and ovaries
Once the childbearing years are finished, hysterectomy may seem a logical treatment option. This is because pregnancy is often considered to be the only function of the uterus, which may explain Australian's high hysterectomy rate. However, the uterus has a number of other important functions, including:
- SEXUALLITY- the uterus rhythmically contracts during orgasm, contributing to sensations of pleasure.
- HORMONE PRODUCTION - some researchers believe the uterus contributes to the maintenance of the female hormonal system. The ovaries also play a major role in maintaining the female hormonal system. Their removal results in instant menopausal symptoms and therefore, unless diseased, they should not be removed during hysterectomy.
- SELF IMAGE - the uterus is of considerable psychological importance, whether or not it is menstruating and capable of bearing a child.
Other treatments
The conditions that prompt a hysterectomy can often be treated by other means. It is recommended that women consider hysterectomy as a procedure of last resort, when all other treatment options have failed. Other options include:
- DRUG TREATMENT - medications may be given to reduce or stop heavy bleeding. This is generally used in the short term to provide symptom relief and to allow women time to explore and consider other treatment options.
- ENDOMETRIAL ABLATION - this involves the removal or stripping of the lining of the uterus, which is shed each month as a period. This procedure requires admission to hospital as a day patient. An anaesthetic is used. Endometrial ablation can successfully reduce or stop heavy bleeding in 85 per cent of cases. It is not recommended for women who wish to become pregnant.
- CONSERVATIVE TREATMENT OF FIBROID - the size, number and position of the fibroids will determine the treatment options offered. Fibroids can be 'shrunk' using medication or by surgery, which burns them away. They can also be starved of a blood supply required for growth, or they can be individually removed through surgery, leaving the uterus intact. Sometimes a combination of these treatments may be advised.
- SURGICAL REMOVAL OF ENDOMETRIOSIS - this involves cutting or burning out tissue deposits and adhesions from such areas as the ovaries, bladder, bowel, uterus, pelvic walls and ligaments which support the uterus. Hormone therapy may be used before or after surgery.
- REMOVAL OF ADENOMYOSIS - localised disease can be excised (cut out) or diathermied (burnt off), leaving the uterus intact. This procedure is recommended for those women who wish to become pregnant. It has a 50 per cent success rate - that is, adenomyosis recurs in approximately one half of cases.
Things to remember
- Hysterectomy is the surgical removal of the womb (uterus), with or without the removal of the ovaries.
- Hysterectomy is used to treat a variety of conditions, including heavy or painful periods, fibroids and prolapse.
- It is recommended that women consider hysterectomy as a procedure of last resort, when all other treatment options have failed.
Labels: Carcinoma, Gynecology, Myoma Uteri, Uterine Bleeding
A myomectomy is an operation performed to remove benign tumours called fibroids from the muscular wall of the uterus.
Fibroids often cause pain and excessive menstrual bleeding. They can also interfere with your ability to become pregnant. They may degenerate or become infected, and therefore your doctor may feel they should be surgically removed.
A hysterectomy may be suggested if you are over childbearing age.
Uterine fibroids
Fibroids are categorised by their locations, which include:
- INTRAMURAL- in the uterine wall. Intramural fibroids are the most common variety.
- SUBMUCOSAL - in the uterine lining (endometrium). This type tends to cause excessive menstrual bleeding and period pain.
- SUBSEROSAL- on the exterior wall of the uterus. They sometimes appear like long stalks.
Medical issues to consider
Your doctor may order an ULTRASOUND SCAN to try to pinpoint the fibroids prior to surgery.
Some BLOOD TESTS may be ordered to see if you are anaemic (symptoms can include excessive tiredness, breathlessness on exertion, pale skin and poor resistance to infection).
A URINE TEST will tell if you have an infection in your urinary system.
The ANAESTHETIST VISITS anaesthetist visits you prior to your operation to see if you are suitable to have a general anaesthetic. (If you are not suitable, you may have the operation performed under a spinal or epidural anaesthetic.) For a general anaesthetic, you are usually given a pre-medication injection to dry up your internal secretions and make you feel drowsy.
Some surgeons request you have an ENEMA and a portion of your pubic hair shaved prior to surgery.
Operation procedure
In most cases, the surgeon performs a DILATATION and CURETTAGE (D&C) to check for irregularities in the inner surface of the uterus. The kind of myomectomy performed depends on the type, size, number and location of the fibroids, but can include:
- ABDOMINAL MYOMECTOMY - the uterus is accessed via one large incision through the abdomen. Usually, a horizontal cut just on the bikini line is performed; in some cases, the incision may need to be made vertically in the midline of your abdomen. The uterus is cut, sometimes with a laser (which closes off blood vessels and reduces bleeding). The fibroids are then removed and the uterus, abdominal wall and skin are closed with sutures. This type of myomectomy is preferred for multiple or deeply rooted fibroids. The drawback of abdominal myomectomy is that it takes longer to recover.
- LAPAROSCOPIC MYOMECTOMY - subserosal fibroids can often be removed via laparoscopic (‘keyhole’) myomectomy. The surgeon makes a number of small incisions, which allow different instruments access to the uterus. Among these instruments is the laparoscope, which contains fibre-optic camera heads or surgical heads (or both). The fibroids are removed, and the small wounds sutured (sewn) closed. Recovery time for the patient is comparatively fast.
- HYSTEROSCOPIC MYOMECTOMY - the fibroids are removed via the dilated cervix, so no abdominal incisions are needed. The instrument is called a resectoscope, which is a hysteroscope fitted with a wire loop. The instrument is inserted through the cervix, and the wire loop slung over the fibroid. Electrical energy passes through the loop, which cuts the fibroid loose. The fibroid can then be removed through the vagina.
| | |
Immediately after the operation
After the operation, you can expect:
- Your temperature, pulse, respiration and blood pressure is observed and noted.
- Any vaginal discharge is noted.
- An intravenous fluid line may still be running into your arm to replace fluids in your body. Antibiotics may be included to combat infection.
- You may have some tubes at the wound site to drain off excess fluid if necessary.
- If you need pain relief, tell your nurse.
- You may have a catheter to drain off urine for the next day or so.
- You are given a normal diet, once your doctor feels it is safe to do so. Tell your nurses as soon as you pass wind or a bowel motion, as this shows that your digestive system is getting back to normal.
- Perform your breathing, coughing and leg exercises hourly when you are awake.
- You are assisted out of bed and taken for a walk the day following surgery.
- You may be in hospital for five to seven days following surgery.
Possible complications
Possible complications of myomectomy include:
- Haemorrhage
- Injury to the uterus
- Damage to the nearby organs of the urinary system
- Formation of scar tissue (adhesions) within the uterus
- Infection
- Blood clots
- Eventual re-growth of fibroids.
Taking care of yourself at home
Be guided by your doctor, but general suggestions include:
- TRY TO REST as much as possible for two weeks.
- Avoid standing for more than a few minutes at a time.
- Continue to TAKE YOUR MEDICATION , and follow strictly the instructions on taking your antibiotics.
- After two weeks, AIM TO WALK for about 10 minutes every day, unless advised otherwise by your doctor.
- Depending on the type of surgery, you can RETURN TO WORK rk within two to six weeks (abdominal myomectomy takes the longest recovery time).
- If you have any excessive vaginal bleeding, or signs of infection at your wound site (such as redness, increasing pain, swelling, or an increased or offensive discharge from your wound), see your doctor immediately.
Long term outlook
You will still have your uterus and all reproductive organs following myomectomy.
Once healed, there should be no effects on your sexual activity, and you should still be able to conceive. Depending on the depth of the scar in your uterus, you may require an elective caesarean section at 38 weeks to safely give birth.
If you are seeking myomectomy as a remedy to excessive menstrual bleeding, it is important to know that the operation is unsuccessful in around 20 per cent of cases - your heavy menstrual flow may be due to factors other than fibroids. See your doctor for further information and advice.
Other forms of treatment
Other possible forms of treatment for fibroids may include:
- MONITORING - if the fibroids are asymptomatic, a ‘wait and see’ approach is often adopted.
- DRUGS - such as hormones, used in combination, to shrink the fibroids prior to surgery.
- HYSTERECTOMY- the surgical removal of some or all of the uterus. Pregnancy is no longer possible after a hysterectomy.
Labels: Gynecology, Myoma Uteri, Uterine Bleeding
UTERINE MYOMA
Fibroids, or myomas, are growths or benign tumours that form inside the uterus (womb). Around four in 10 women over the age of 40 will have fibroids.
No one knows why fibroids develop, but it is suspected that the sex hormones – oestrogen and progesterone – play significant roles. This is because fibroids rarely grow in prepubescent girls and postmenopausal women.
Pre-existing fibroids stop growing, and may even shrink, once a woman passes the menopause.
Fibroids often cause no problems, but may occasionally be associated with infertility, miscarriage and premature labour. Other possible problems include heavy, lengthy and painful periods. Treatment depends on the size, number and location of the fibroids, but may include drugs, procedures performed under local anaesthetic and surgery. Fibroids rarely turn cancerous.
Symptoms
Most women with fibroids have no symptoms. When present, symptoms may include:
- Heavy periods
- Lengthy periods
- Period pain
- Spotting between periods
- Painful intercourse
- A sensation of heaviness or pressure in the back, bowel and bladder
- Frequent urination
- A lump or swelling in the lower abdomen.
Different types
Fibroids are categorised by their location, which includes:
- INTRAMURAL – growing in the uterine wall. Intramural fibroids are the most common variety.
- SUBMUCOSAL– growing in the uterine lining (endometrium). This type tends to cause excessive menstrual bleeding and period pain.
- SUBSEROSAL – growing on the exterior wall of the uterus. These sometimes appear like long stalks.
Common complications
Fibroids can cause a variety of complications, including:
- ANEMIA – excessive menstrual blood loss can cause anaemia, a disorder characterised by the body’s inability to carry sufficient oxygen in the blood. Symptoms of anaemia include breathlessness, fatigue and paleness.
- URINATION PROBLEMS– large fibroids can bulge the uterus against the bladder, causing a sensation of fullness or discomfort and the need to urinate often.
- INFERTILITY – the presence of fibroids can interfere with implantation of the fertilised egg in a number of ways. For example, the egg may try to burrow into a fibroid, or fibroids close to the uterine cavity may ‘prop open’ the uterus, making successful implantation difficult.
- MISCARRIAGE and PREMATURE DELIVERY – fibroids can reduce blood flow to the placenta or may compete for space with the developing baby.
Diagnosis
Uterine fibroid (right lateral wall)
Nine (9) weeks and 4 days gestation
Fibroids can be detected using an ULTRASOUND , where sound waves create a two-dimensional picture.
The inside of the uterus can be examined with a HYSTEROSCOPE , which is a thin tube passed through the cervix (neck of the womb). A small camera may be placed at the tip of the hysteroscope, so that the interior of the uterus can be viewed on a monitor.
Treatment
Treatment depends on the location, size and number of the fibroids, but may include:
- MONITORING – if the fibroids are causing no symptoms and are not large, a ‘wait and see’ approach is usually adopted.
- DRUGS– such as hormones, used in combination to shrink the fibroids prior to surgery.
- ARTERIAL EMBOLISATION – under local anaesthetic, a fine tube is passed via an artery in the arm or leg into the main artery supplying the fibroid with blood. The whole process is monitored by x-ray. Fine particles (like sand) are then injected into the artery to block the blood supply to the fibroid. The fibroid slowly dies and symptoms should settle over a few months.
- HYSTEROSCOPY – the fibroids are removed via the cervix, using a hysteroscope.
- LAPAROSCOPY – or ‘keyhole surgery’, where a thin tube is inserted through the abdomen to remove the fibroids.
- OPEN SURGERY– larger fibroids need to be removed via an abdominal incision. This procedure weakens the uterine wall and makes Caesarean sections for subsequent pregnancies more likely.
- HYSTERECTOMY – the surgical removal of some, or all, of the uterus. Pregnancy is no longer possible after a hysterectomy.
Labels: Gynecology, Uterine Bleeding
Gonorrhoea
Gonorrhoea is caused by bacteria known as Neisseria gonorrhoeae.
It usually affects the genital area, although the throat or anus (back passage) may also be involved.
Gonorrhoea affects both men and women and is easily transmitted during vaginal intercourse. It can also be transmitted during anal or oral sex.
Gonorrhoea may not cause symptoms in women
A lack of specific signs and symptoms means gonorrhoea may go undetected for longer in women. Often there are no symptoms. Sometimes, gonorrhoea causes:- An unusual discharge from the vagina
- Pain while urinating or passing water.
Untreated gonorrhoea can lead to infertility in women
If left untreated, gonorrhoea can lead to pelvic inflammatory disease (PID), which can cause infertility. Symptoms of PID include:- Lower abdominal pain and tenderness
- Deep pain during sexual intercourse
- Heavy and painful periods
- Fever.
A check for gonorrhoea may be recommended
 Because gonorrhoea may not cause symptoms until PID has already developed, sexually active women who have recently had a change of sexual partner or feel they may be at risk of a sexually transmissible infection (STI) should have a test for gonorrhoea (and for chlamydia infection).
Because gonorrhoea may not cause symptoms until PID has already developed, sexually active women who have recently had a change of sexual partner or feel they may be at risk of a sexually transmissible infection (STI) should have a test for gonorrhoea (and for chlamydia infection).Men may experience a burning sensation while urinating
Gonorrhoea commonly infects the inside of the penis (the urethra). Symptoms may include:
- A burning sensation while urinating or passing water
- A white or yellow pus-like discharge from the penis
- Swelling and pain in the testicles, which can occur if the gonorrhoea infection goes untreated.
Oral and anal gonorrhoea
 In both men and women:
In both men and women: - ANAL GONORRHOEA Anal gonorrhoea often occurs without signs or symptoms
- THROAT GONORRHOEA may cause a sore throat, however, it usually occurs without symptoms.
Gonorrhoea is treated with antibiotics
Gonorrhoea is treated with antibiotics. Some strains of gonorrhoea are now resistant to penicillin and some other antibiotics. Tell your doctor if you have been travelling overseas because many of the new resistant strains have originated from outside Australia.Prevention through the proper use of condoms and dams is best
The best protection against gonorrhoea is to always use barrier protection such as condoms, female condoms and dams (a thin piece of latex placed over the anal or vulval area during oral sex). Condoms and dams can be used for oral-vaginal sex and oral-anal sex to help prevent the spread of infection.
Condoms for men can be bought from supermarkets, chemists and other outlets. Female condoms and dams are available through Family Planning Victoria and may be available from selected shops. Latex free condoms are also available from some outlets. Male condoms and lubricant are available free from the Melbourne Sexual Health Centre, along with female condoms and dams on request.
When using a condom for men you should:
- Open the packet carefully so that you don’t tear the condom.
- Pinch the tip of the condom before carefully rolling it down the entire shaft of the erect penis.
- Do not use spit, Vaseline, baby oil or other oil-based lubricants.
- Use water-based lubricants, such as KY, Muko or Wet Stuff.
- Withdraw the penis before the erection is lost, so that the condom does not fall off. Hold the base of the condom to prevent spills.
- Store condoms in a cool, dry place and check the expiry date.
Salpingitis

Salpingitis is inflammation of the fallopian tubes. Almost all cases are caused by bacterial infection, including sexually transmitted diseases such as gonorrhoea and chlamydia. The inflammation prompts extra fluid secretion or even pus to collect inside the fallopian tube. Infection of one tube normally leads to infection of the other, since the bacteria migrates via the nearby lymph vessels.
Salpingitis is one of the most common causes of female infertility. Without prompt treatment, the infection may permanently damage the fallopian tube so that the eggs released each menstrual cycle can't meet up with sperm. Treatment options include antibiotics. Salpingitis is sometimes called pelvic inflammatory disease (PID). This umbrella term includes other infections of the female reproductive system, including the uterus and ovaries.
Symptoms
In milder cases, salpingitis may have no symptoms. This means the fallopian tubes may become damaged without the woman even realising she has an infection. The symptoms of salpingitis may include:
- Abnormal vaginal discharge, such as unusual colour or smell
- Spotting between periods
- Dysmenorrhoea (painful periods)
- Pain during ovulation
- Uncomfortable or painful sexual intercourse
- Fever
- Abdominal pain on both sides
- Lower back pain
- Frequent urination
- Nausea and vomiting
- The symptoms usually appear after the menstrual period.
Acute and chronic salpingitis
Salpingitis is usually categorised as either acute or chronic. In acute salpingitis, the fallopian tubes become red and swollen, and secrete extra fluid so that the inner walls of the tubes often stick together. The tubes may also stick to nearby structures such as the intestines. Sometimes, a fallopian tube may fill and bloat with pus. In rare cases, the tube ruptures and causes a dangerous infection of the abdominal cavity (peritonitis). Chronic salpingitis usually follows an acute attack. The infection is milder, longer lasting and may not produce many noticeable symptoms.
Most cases are caused by bacteria
In nine out of 10 cases of salpingitis, bacteria are the cause. Some of the most common bacteria responsible for salpingitis include:
- Chlamydia
- Gonococcus (which causes gonorrhoea)
- Mycoplasma
- Staphylococcus
- Streptococcus.
Access to the reproductive system
The bacteria must gain access to the woman's reproductive system for infection to take place. The bacteria can be introduced in a number of ways, including:
- Sexual intercourse
- Insertion of an IUD (intra-uterine device)
- Miscarriage
- Abortion
- Childbirth
- Appendicitis.
Lifestyle risk factors
Lifestyle factors that significantly increase a woman's risk of contracting salpingitis include:
- Engaging in sexual intercourse without a condom
- Prior infection with a sexually transmitted disease.
Complications of salpingitis
Without treatment, salpingitis can cause a range of complications, including:
- FURTHER INFECTION - the infection may spread to nearby structures, such as the ovaries or uterus.
- INFECTION OF SEX PARTNERS - the woman's partner or partners may contract the bacteria and become infected too.
- TUBO-OVARIAN ABSCESS - about 15 per cent of women with salpingitis develop an abscess, which requires hospitalisation.
- ECTOPIC PREGNANCY - a blocked fallopian tube prevents the fertilised egg from entering the uterus. The embryo then starts growing inside the confined space of the fallopian tube. The risk of ectopic pregnancy for a woman with prior salpingitis or other form of pelvic inflammatory disease (PID) is around one in 20.
- INFERTILITY - the fallopian tube may become deformed or scarred to such an extent that the egg and sperm are unable to meet. After one bout of salpingitis or other PID, a woman's risk of infertility is about 15 per cent. This rises to 50 per cent after three bouts.
Diagnosis methods
Diagnosing salpingitis involves a number of tests, including:
- GENERAL EXAMINATION - to check for localised tenderness and enlarged lymph glands.
- PELVIC EXAMINATION - to check for tenderness and discharge.
- BLOOD TESTS - to check the white blood cell count and other factors that indicate infection.
- MUCUS SWAB - a smear is taken to be cultured and examined in a laboratory so that the type of bacteria can be identified.
- LAPAROSCOPY - in some cases, the fallopian tubes may need to be viewed by a slender instrument inserted through abdominal incisions.
Treatment options
Treatment depends on the severity of the condition, but may include:
- ANTIBIOTICS - to kill the infection, which is successful in around 85 per cent of cases.
- HOSPITALISATION - including intravenous administration of antibiotics.
- SURGERY- if the condition resists drug treatment.
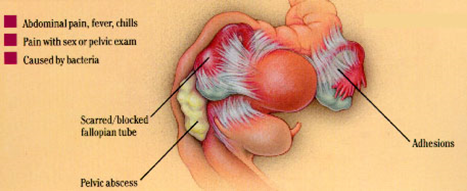
Pelvic Inflammatory Disease – PID
Pelvic inflammatory disease (PID) occurs when an infection spreads from the vagina to the cervix, endometrium (lining of the uterus) and fallopian tubes. The infection is usually sexually transmitted. It can also occur after a ruptured (burst) appendix or a bowel infection.
Some surgical procedures, such as abortion or insertion of an intrauterine device (IUD), can lead to PID.
The infection usually occurs in three stages - the cervix is infected first, followed by the endometrium and then the fallopian tubes.
The silent epidemic
PID is often called the ‘silent epidemic’ because it is common among sexually active women but does not always cause symptoms. About 10,000 women in Australia are treated for PID in hospital each year. About 10 to 30 times that number are treated as outpatients. Women aged 20 to 29 have the highest reported incidence of PID.
Signs and symptoms that can occur
Signs and symptoms of PID that may occur include:
- Lower abdominal pain or tenderness
- Menstrual disturbances
- Burning pain when urinating (dysuria)
- A change in smell, colour or amount of vaginal discharge
- Deep pain during sexual intercourse
- Fever.
Female infertility can be a devastating consequence
Scarring and blockage of the fallopian tubes is the most frequent long term complication of PID. Infertility occurs because the fertilised egg cannot pass through the tube to the uterus:
- One episode of PID doubles the risk of tubal infertility.
- The risk of fallopian tube blockage rises to 75 per cent after three or more episodes of PID.
- The risk of ectopic pregnancy (where the foetus develops outside the uterus) after one episode of PID is increased seven fold.
Chlamydia and gonorrhoea are the most common causes of PID
Chlamydia is responsible for 50 per cent of PID cases while gonorrhoea is the cause in 25 per cent of cases. The risk of fallopian tube blockage is slightly higher for PID caused by gonorrhoea. Both are bacterial infections and are sexually transmitted diseases (STDs). Non-specific urethritis, the most common STD among men, is most often caused by chlamydia.
Diagnosing PID
Your doctor will test for possible causes like chlamydia and gonorrhoea. In some cases, laparoscopy is required to correctly diagnose PID. Laparoscopy involves inserting an endoscope (which is like a surgical video camera) into the abdomen to view the reproductive organs.
Without treatment, chronic pain may develop
Chronic pain and, sometimes, severe disability can occur if PID is not treated. This is usually due to extensive scarring. Treatment involves:
- ANTIBIOTICS that are active against a broad range of organisms - amoxycillin (a type of penicillin) and doxycycline are usually prescribed.
- TESTING and TREATING male partners and treating them, if necessary - symptoms may be mild or non-existent in men.
- AVOIDING GENITAL SEXUAL XONTACT until the treatment is complete and a negative test result is obtained.
- SURGERY to remove scar tissue.
Protecting yourself from PID
To help prevent the transmission of the bacteria that can cause PID:
- Use condoms during vaginal or anal intercourse.
- Use condoms if you have an intrauterine device (IUD) inserted.
Use of the oral contraceptive pill may help
Sexually active women who are on the pill appear to have only one-third the risk of PID compared to women not on the pill. However, this data was collected in the 1970s and it is not known if the lower-dose pills more commonly used now have the same protective effect, although it is likely that they do.
The tissue that lines the interior of the uterus is called the endometrium.
Endometriosis is the growth of endometrial tissue (from the lining of the uterus) in places outside of the uterus, such as the ovaries, fallopian tubes and bowel.
Endometriosis can cause numerous symptoms, including painful periods and pain with sex, fertility problems, pelvic and ovulation pain, pain in the lower back and thighs, and bowel and bladder symptoms.
Treatment options include :
- SURGERY
- HORMONE TRATMENT and
- COMPLEMENTARY THERAPIES
Diagnosis can be difficult
Diagnosing endometriosis can be difficult, especially in the early stages of disease. The only way to diagnose the disease is to look inside the pelvic cavity, using a special instrument called a laparoscope. Diagnosis may be delayed if the woman assumes her degree of pain is normal and so doesn’t see her doctor. A diagnosis may also be delayed if the doctor is not familiar with the range of symptoms associated with endometriosis. If you have bad period pain, you should see your doctor.
Treatment options
The treatment options for endometriosis include:
- Observation with no medical intervention
- Hormone treatment
- Surgery
- Combined treatment
- Complementary therapies.
Observation with no medical intervention
In mild cases of endometriosis, it may be possible to simply monitor the condition with regular visits to your doctor or gynaecologist. Antiprostaglandin medications (non-steroidal anti-inflammatory drugs such as ibuprofen and mefenamic acid) can help to control any associated pain.
If symptoms progress, talk over the medical options with your health care provider before making a final decision. Remember that a mild condition can become moderate to severe. Removal of adhesions through surgery is the most effective treatment to lessen the chances of recurrence.
Hormone treatment
Each month, a woman’s uterine lining is prompted by the hormone oestrogen to thicken in preparation for possible pregnancy. During menstruation, the hormone progesterone causes the plump uterine lining to shed. The misplaced endometrial cells in other areas of the body also respond to oestrogen and progesterone. Hormone therapy can sometimes be an effective way to manage the symptoms of endometriosis.
Options for hormone therapy include:
- GESTRINONE – is a synthetic hormone that causes the endometriosis to become inactive and waste away. Side effects of gestrinone include weight gain, acne, depression, mood swings, hot flushes and loss of libido (sex drive).
- DYDROGESTERONE– a synthesised version of the hormone progesterone, which helps to dry up the stray endometrial cells. Ovulation may still occur. Side effects of dydrogesterone can include depression, tender breasts, weight gain, fatigue, nausea, headaches and dizziness.
- MEDROXYPROGESTERON ACETATE– another synthesised version of the hormone progesterone. Most women taking medroxyprogesterone acetate will stop ovulating and menstruating. Other side effects include weight gain, bloating, irregular vaginal bleeding, depression, sweating, headaches, acne, nausea, fatigue and tender breasts.
- GnRH AGONIST– gonadotrophin-releasing hormones help to govern the menstrual cycle. GnRH agonists are drugs that stop the ovaries from producing as much oestrogen by reducing the hormones produced by the pituitary gland (follicle stimulating hormone and luteinising hormone). Without oestrogen, the misplaced endometrial cells are unable to grow. Side effects of GnRH agonists include menopausal symptoms such as thinning of the bones, hot flushes, dry vagina, headaches, depression, loss of libido and night sweats. These symptoms can be relieved, while still maintaining the benefit of the treatment, by adding back oestrogen and progesterone.
- The oral CONTRACEPTIVE PILL– the pill is frequently used to achieve long-term suppression of endometriosis. It can be used to stop the disease progressing in women with mild disease or to stop the disease from recurring following surgical or hormonal treatment.
- DANAZOLE– this mild form of the male hormone testosterone reduces the amount of oestrogen produced by the ovaries to around the same level as occurs during menopause. Without oestrogen, the stray endometrial cells can’t grow and, therefore, shrink and disappear during the treatment. Danazol is now rarely used to treat endometriosis due to its serious side effects, which can include weight gain, bloating, fluid retention, acne, smaller breasts, increase in muscle mass, increased facial and body hair, muscle cramps, mood swings, voice deepening and clitoral enlargement. Danazol can also cause gastrointestinal upsets, depression and liver disease. These treatments can have side effects, so make sure you are well informed about them before you and your doctor decide on your treatment.
Surgery
The different types of surgery include:
- LAPAROSCOPIC SURGERY– a slender tube is inserted into the abdominal cavity via a small incision (also known as ‘keyhole’ surgery). Endometrial implants, cysts and adhesions are then removed by cutting out (excision), burning (cauterisation) or vapourising (ablation) them. Cutting out is the most effective of these methods. You should seek an expert in advanced laparoscopic surgery to conduct your procedure. Some doctors can perform surgery, including the removal of the ovaries or removal of endometriosis from the bowel, laparoscopically.
- LAPAROTOMY (open surgery) – a surgical incision into the abdominal cavity to cut out or burn tissue or remove cysts (with the advent of laparoscopic surgery, this procedure is now rarely necessary).
- BOWEL RESECTION – may be necessary if the bowel has developed endometriosis adhesions.
- HYSTERECTOMY – the uterus is removed, along with endometrial implants, cysts and adhesions. In some cases, the fallopian tubes and ovaries will also be removed. Unfortunately, hysterectomy does not always cure endometriosis.
Combined treatment
In some cases, a woman will benefit from undergoing hormone therapy as well as surgery. Hormone therapy may be offered before or after the surgery, depending on the circumstances.
Complementary therapies
Some women find complementary therapies to be helpful. Always tell your doctor about the kinds of complementary therapies you are using or considering. Options include:
- Acupuncture
- Chinese medicine
- Herbal therapy
- Homeopathy.
Pregnancy is not a cure
Some people believe that endometriosis can be cured by pregnancy. This isn’t the case. The symptoms may improve for some women, but worsen in others. For those women who experience an end to all symptoms during pregnancy, the relief may only be short lived. Unfortunately, for some women, the endometriosis will recur.
Labels: Dysmenorrhoea, Endometriosis, Infertility
The tissue that lines the inside of the uterus is called the endometrium. Endometriosis is the growth of endometrial tissue in places outside the uterus, such as the ovaries, uterus, bowel and lining of the pelvic cavity.
The causes of endometriosis remain unknown, but researchers have uncovered a number of possible causes and risk factors.
Endometriosis can cause numerous symptoms, including :
- Painful periods (DYSMENORRHOEA)
- Pain with sex (DYSPAREUNIA) ,
- Fertility problems,
- Pelvic and ovulation pain,
- Pain in the lower back and thighs, and
- Bowel and bladder symptoms.
Usually, endometriosis causes pain around the time of the period, but some women experience almost constant pain. If you have bad period pain, you should see your doctor.
Stray endometrial cells respond to hormones
The endometrium responds to the sex hormones oestrogen and progesterone. In women with endometriosis, the stray endometrial cells in the pelvic cavity also respond to these hormones.
During ovulation, oestrogen prompts the uterine lining – and the misplaced endometrial cells – to thicken. However, the misplaced endometrial cells cannot leave the body via menstruation; they simply bleed a little, causing inflammation and pain, and then heal. Over time, this may create scar tissue. Affected organs, such as the ovaries and bowel, may stick together. This can cause chronic pain and bowel symptoms. Sometimes, it can cause fertility problems if the scar tissue (adhesions) stops the released egg from getting to the fallopian tube.
Genetic susceptibility
Studies indicate that some women are genetically predisposed to developing endometriosis. According to researchers from the University of Queensland, endometriosis runs in families, which means the genetic susceptibility is inherited.
Australian researchers have found that women who have a sister with the disease are 2.3 times more likely to have the disease than women in the general community. The increased likelihood of developing the disease is not just confined to the daughters and sisters of women with the disease but also affects their cousins.
Possible causes
Some of the theories on what causes endometriosis include:
- Retrograde menstruation
- Immune system malfunction
- Genetic factors.
Retrograde menstruation
Retrograde menstruation is also known as ‘backward menstruation’. The lining of the uterus is shed during the period. In almost all women, some of the menstrual fluid flows backwards into the fallopian tubes instead of leaving the body through the vagina.
Since the fallopian tubes are open-ended (they are not joined to the ovaries, but open nearby), menstrual fluid can drip into the pelvic cavity. It is suspected that, in women who experience endometriosis, the endometrial tissue contained in the menstrual fluid sticks to whatever structures it lands on (such as the ovaries) and starts to grow.
Immune system malfunction
Retrograde menstruation occurs in almost all women, but only 3–10 per cent of menstruating women develop endometriosis. One theory suggests that the immune systems of some women allow endometriosis to develop by failing to control or stop the growth of endometrial tissue outside the uterus.
The genetic factor
It seems that genetic susceptibility plays a significant role in the development of endometriosis – but how? Some researchers suspect that some families carry faulty genes that allow abnormal cells to survive and grow in the pelvic cavity.
Risk factors
Apart from genetic susceptibility, some of the suspected risk factors include:
- MENSTRUAL CYCLE FACTORS– some evidence suggests that women with endometriosis are more likely to have started their periods at an early age. Other factors related to the menstrual cycle that may predispose a woman to endometriosis include heavy or painful periods, short menstrual cycles (less than 27 days) and long periods (more than one week).
- ALLERGIES – such as food, eczema and hay fever.
- OBESITY
- EXPOSURE TO TOXINS – persistent environmental pollutants, such as dioxins, are suspected of contributing to the development of endometriosis. Animal experiments have indicated such an effect, but at levels of exposure higher than those currently seen in humans.
Reducing your endometriosis risk
Factors that may help reduce your risk of endometriosis include:
- AEROBIC EXCERCISE of five hours per week – studies show a 50 per cent reduction in the risk of recurrence
- CHILDBEARING – reduces the risk of recurrence by about 50 per cent.
- The CONTRACEPTIVE PILL – this prevents ovulation, during which there is a surge of oestrogen production and spill into the pelvis.
Labels: Dysmenorrhoea, Endometriosis, Infertility
Endometriosis is a condition in which endometrium, the tissue that normally lines the womb (uterus), grows in locations outside the uterus.
Endometriosis may cause adhesions (fibrous scar tissue) on the uterus.
The uterus can become stuck to the ovaries, fallopian tubes and bowel.
The pain of endometriosis can be so bad that it stops you from going to work or school. Usually, it causes pain around the time of your period but for some women the pain is almost constant. If you need treatment, you may need emotional as well as physical support.
Symptoms
The symptoms of endometriosis include:
- Painful periods
- Pain with sex
- Pelvic pain
- Ovulation pain
- Pain in the lower back and thighs
- Bowel symptoms
- Bladder symptoms
- Reduced fertility
- Nausea and lethargy
- Pre-menstrual tension (PMT).
Many women think that painful periods are normal. If you have bad period pain, you should see your doctor.
Diagnosis
Tests that are used to help diagnose endometriosis include:
- LAPAROSCOPY– surgical procedure performed under general anaesthetic, where a medical instrument with a video camera attached is used to examine your pelvic organs.
- ULTRASOUND – a vaginal or abdominal instrument that uses sound waves to create a video image of your pelvic organs.
- COLONOSCOPY– a medical instrument with a video camera attached that is used to examine your bowel. This is done if it is thought that the endometriosis could also be affecting your bowel. You would be sedated for the procedure.
Endometriosis may not show up during an internal pelvic examination. Your doctor may need to refer you to a gynaecologist if you have endometriosis.
Treatment
Endometriosis can be treated medically (with drugs or medicine) or with surgery. Sometimes both medicine and surgery are used. Some women also benefit from natural therapies.
Drug therapy
Medications that are used to help treat endometriosis include:
- Anti-inflammatory medications
- Pain killers (Mersyndol is often used)
- Hormonal treatments, which suppress ovulation and menstruation and may have side effects. There are different categories of these such as GnRH agonists (Zoladex, Synarel), androgenic steroids (Danocrine, Azol, Dimetriose), progestogens (Provera, Duphaston, Primolut) and the oral contraceptive pill.
Surgery
Surgical methods used to treat endometriosis include:
- LAPAROSCOPIC SURGERY– performed to diagnose and treat endometriosis. Laser surgery may be used to remove the adhesions. This is done to reduce pain and improve the chances of you becoming pregnant.
- LAPAROTOMY – to cut out or burn tissue or remove cysts.
- BOWEL RESECTION – may be necessary if the bowel has developed endometriosis adhesions.
- HYSTERECTOMY(removal of the uterus) – may be an option if endometriosis is significantly impacting on your quality of life and other treatments have not worked.
If your ovaries are removed during a hysterectomy, you will need to discuss hormone replacement with your doctor.
Complementary therapies
There are many different forms of complementary therapies that can be used to treat endometriosis. Most therapies may be used in conjunction with Western medicine or instead of surgery and drug therapy.
Examples of different therapies include:
- Herbal medicine
- Homeopathy
- Traditional Chinese medicine
- Nutritional therapies
- Massage
- Yoga.
Labels: Dysmenorrhoea, Endometriosis, Infertility
Sunday, November 29, 2009
Adenomyosis
Known as "Endometriosis of the uterus," Adenomyosis is benign and does not cause cancer. Most commonly, the disease affects the back wall (posterior side) of the uterus. The endometrial cells penetrate deep into the uterine muscle (myometrium). When this occurs, the uterus is enlarged usually more than twice the normal size and very hard. The disease may be localized with well-defined borders or diffuse, meaning having no limits or borders. When this localized disease is found it is called adenomyoma. These adenomyomas can be located at different depths of the uterine muscle and can penetrate into the uterine cavity, becoming submucosal tumors
How common is Adenomyosis?
This disease can only be diagnosed with 100% certainty by doing a biopsy of the uterine muscle. Depending on the various reported studies published, it has been noted to occur in 8-62% of women who have had hysterectomies. 12% of women with Adenomyosis have also had Endometriosis in other sites such as the pelvic wall, ovaries, fallopian tubes etc. The highest incidence is seen in women in their mid to upper forties, and though this disease may cause infertility, it often appears in women who have already had children.
What are the symptoms of Adenomyosis?
As with Endometriosis, patients with Adenomyosis may not show any symptoms (asymptommatic). However, women most commonly experience excessive, heavy or prolonged menstrual bleeding and painful periods (dysmenorrhea). The amount of bleeding and cramps is usually associated with the degree of disease involvement and depth of penetration into the uterine walls. Extensive involvement of the uterine muscle can also interfere with the normal contractility of the muscle which then leads to excessive bleeding.
How is Adenomyosis diagnosed?
An exact diagnosis is often difficult to establish pre-operatively because abnormal patterns of bleeding (dysfunctional bleeding) and fibroid tumors can result in similar symptom patterns. Sometimes during a D&C procedure to remove intra-uterine polyps or small fibroid tumors, tissue is removed enabling a pathologist to make the diagnosis.
Pelvic Exam Findings
Pelvic exam findings can reveal a normal, or only slightly enlarged uterus to a very firm tender uterus enlarged to twice the normal size.
MRI- Magnetic Resonance Imaging
At times, this can distinguish adenomyomas from fibroid tumors, but again, experienced physicians and radiologists possessing extensive training are required.
MRI provides better diagnostic capability due to the increased spatial and contrast resolution, and to not being limited by the presence of bowel gas or calcified uterine fibroids (as is ultrasound). In particular, MR is better able to differentiate adenomyosis from multiple small uterine fibroids. The uterus will have a thickened junctional zone with diminished signal on both T1 and T2 weighted sequences due to susceptibility effects of iron deposition due to chronic microhemorrhage. A thickness of the junctional zone greater than 10 to 12 mm (depending on who you read) is diagnostic of adenomyosis (<8 mm is normal). Interspersed within the thickened, hypointense signal of the junctional zone, one will often see foci of hyperintensity (brightness) on the T2 weighted scans representing small cystically dilatated glands or more acute sites of microhemorrhage.
MR can be used to classify adenomyosis based on the depth of penetration of the ectopic endometrium into the myometrium.
Transvaginal Ultrasound
Extensive recent work has been completed with this test, but the amount of false positive results is still high.
Tissue Diagnosis
Tissue diagnosis in some form remains the only definitive method for diagnosing Adenomyosis. If the diagnosis is suspected pre-operatively, then a laparoscopy and a long needle biopsy can be performed, whereby a needle is inserted into the back of the uterus to collect a tissue sample for pathological testing. It may also be diagnosed when fibroid tumors are removed .
Can Adenomyosis be treated without surgery?
Some studies have shown that there is a relationship between Adenomyosis and hormone imbalance, most commonly an excess of estrogen. Progesterone therapy, either in the natural or synthetic form has been known to help, but shows very little long term benefits. A medication called Danazol may be helpful in treating the pain and decreasing the size of the uterus but long term positive results are poor. Although gonadotropin-releasing hormone agonists such as Lupron have been found to reduce uterine symptoms of adenomyosis during treatment, the symptoms return quickly after the medicine wears off.
How can Female Alternative Surgery help Adenomyosis?
Most commonly, hysterectomy has been the mainstay of treatment. Traditional medicine states that since most women with Adenomyosis are beyond child-bearing age, the uterus is no longer relevant. At the Institute, we want to give women every opportunity to retain their female organs even if fertility is not a concern. Our surgical approach is first to make a diagnosis. For women who still wish to conceive, we try to remove the Adenomyosis using laser technology (CO2 Yag and Argon) which preserves the endometrial cavity but treats the remaining deep uterine muscle disease. In the case of women who are not concerned with fertility but want to preserve their organs, our approach is to remove as much of the affected tissue and, if necessary, decrease the size of the endometrial cavity. We treat the remaining uterine muscle with a deep tissue laser technique. Post surgical results have shown that pain almost always disappears and menstrual flow and volume decrease.
Labels: Dysmenorrhoea, Endometriosis, Infertility
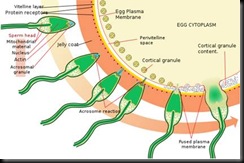
The acrosome reaction for a sea urchin, a similar process. Note that the picture shows several stages of one and the same spermatozoon - only one penetrates the ovum
Human fertilization is the union of a human egg and sperm, usually occurring in the ampulla of the uterine tube. It is also the initiation of prenatal development. Scientists discovered the dynamics of human fertilization in the nineteenth century.[1]
Fertilization (also known as conception, fecundation and syngamy), is the fusion of gametes to produce a new organism. The process involves a sperm fusing with an ovum, which eventually leads to the development of an embryo.
It is when first of all the acrosome at the head tip produces enzymes, which cuts through the outer jelly coat of the egg. After that has happened, the sperm plasma fuses with the egg’s plasma membrane. Finally, the Head disconnects with the body, and the egg can now travel down the Fallopian tube to reach the womb, where the baby grows.
Fertilization may or may not involve sexual intercourse. In vitro fertilisation (IVF) is a process by which egg cells are fertilized by sperm outside the womb, in vitro. Sperm is propelled through the female reproductive tract by flagellation and may get through the jelly coat through a process called sperm activation. The oocyte and sperm fuse once the sperm is through the corona radiata and the zona pellucida; two layers covering and protecting the oocyte from fertilization by more than one sperm.
Corona radiata
Human ovum examined fresh in the liquor folliculi. The zona pellucida is seen as a thick clear girdle surrounded by the cells of the corona radiata.
The egg itself shows a central granular deutoplasmic area and a peripheral clear layer, and encloses the germinal vesicle, in which is seen the germinal spot.
The egg binds the sperm through the corona radiata, a layer of follicle cells on the outside of the secondary oocyte. Fertilization is when the nuclei of a sperm and an egg fuse. The successful fusion of gametes form a new organism.
Acrosome reaction
The acrosome reaction must occur to mobilise enzymes within the head of the spermatozoon to degrade the zona pellucida.
Zona pellucida
The sperm then reaches the zona pellucida, which is an extra-cellular matrix of glycoproteins. A special complementary molecule on the surface of the sperm head then binds to a ZP2 glycoprotein in the zona pellucida. This binding triggers the acrosome to burst, releasing enzymes that help the sperm get through the zona pellucida.
Some sperm cells consume their acrosome prematurely on the surface of the egg cell, facilitating for other surrounding sperm cells, having on average 50% genome similarity, to penetrate the egg cell.[2] It may be regarded as a mechanism of kin selection.
Recent studies have shown that the egg is not passive during this process.[3][4]
Cortical reaction
Once the sperm cells find their way past the zona pellucida, the cortical reaction occurs: cortical granules inside the secondary oocyte fuse with the plasma membrane of the cell, causing enzymes inside these granules to be expelled by exocytosis to the zona pellucida. This in turn causes the glyco-proteins in the zona pellucida to cross-link with each other, making the whole matrix hard and impermeable to sperm. This prevents fertilization of an egg by more than one sperm.
Fusion
After the sperm enters the cytoplasm of the oocyte, the cortical reaction takes place, preventing other sperm from fertilizing the same egg. The oocyte now undergoes its second meiotic division producing the haploid ovum and releasing a polar body. The sperm nucleus then fuses with the ovum, enabling fusion of their genetic material.
Cell membranes
The cell membranes of the secondary oocyte and sperm fuse together.
Transformations
Both the oocyte and the sperm go through transformations, as a reaction to the fusion of cell membranes, preparing for the fusion of their genetic material.
The oocyte now completes its second meiotic division. This results in a mature ovum. The nucleus of the oocyte is called a pronucleus in this process, to distinguish it from the nuclei that are the result of fertilization.
The sperm's tail and mitochondria degenerate with the formation of the male pronucleus. This is why all mitochondria in humans are of maternal origin.
Replication
The pronuclei migrate toward the center of the oocyte, rapidly replicating their DNA as they do so to prepare the new human for its first mitotic division.
Mitosis
The male and female pronuclei don't fuse, although their genetic material do so. Instead, their membranes dissolve, leaving no barriers between the male and female chromosomes. During this dissolution, a mitotic spindle forms around them to catch the chromosomes before they get lost in the egg cytoplasm. By subsequently performing a mitosis (which includes pulling of chromatids towards centrioles in anaphase) the cell gathers genetic material from the male and female together. Thus, the first mitosis of the union of sperm and oocyte is the actual fusion of their chromosomes.
Each of the two daughter cells resulting from that mitosis have one replica of each chromatid that was replicated in the previous stage. Thus, they are genetically identical.
In other words, the sperm and oocyte don't fuse into one cell, but into two identical cells.
Footnotes
- ^ Garrison, Fielding. An Introduction to the History of Medicine, pages 566-567 (Saunders 1921).
- ^ Sleek, Fast and Focused: The Cells That Make Dad Dad New York Times 2007/06/12
- ^ Suzanne Wymelenberg, Science and Babies, National Academy Press, page 17
- ^ Richard E. Jones and Kristin H. Lopez, Human Reproductive Biology, Third Edition, Elsevier, 2006, page 238
Introduction
Most women equate a missed menstrual period with the possibility of being pregnant, but other symptoms and signs are experienced by most women in the early stages of pregnancy. It's important to remember that not all women will experience all of these symptoms or have the symptoms to the same degree. Even the same woman can have different types of symptoms in a subsequent pregnancy than she had in previous pregnancies. The following are the most common pregnancy symptoms in the first trimester.
Missed period
A missed menstrual period is most often the first sign of pregnancy. Sometimes a woman who is pregnant may still experience some bleeding or spotting around the time of the expected period, typically 6 to 12 days after conception. When it occurs, this so-called "implantation bleeding" is generally not as heavy or long as a regular menstrual period. This small amount of bleeding that occurs at the time of the expected menstrual period happens when the fertilized egg attaches to the uterine wall and is referred to as implantation bleeding.
Any bleeding during pregnancy is typically lighter than that observed during the regular menstrual period. However, if a woman does not have regular menstrual cycles, she may notice some of the other symptoms of early pregnancy before it is apparent that the menstrual period has been missed. A missed menstrual period also does not confirm that a woman is pregnant even if she has regular cycles, since both emotional and physical conditions may cause absent or delayed periods.
Breast swelling, tenderness, and pain
Feelings of breast swelling, tenderness, or pain are also commonly associated with early pregnancy. These symptoms are sometimes similar to the sensations in the breasts in the days before an expected menstrual period. Women may also describe a feeling of heaviness or fullness in the breasts. These symptoms can begin in some women as early as one to two weeks after conception.
Nausea and vomiting
Nausea and vomiting are also common in early pregnancy. Traditionally referred to as "morning sickness," the nausea and vomiting associated with early pregnancy can occur at any time of the day or night. Its typical onset is anywhere between the 2nd and 8th weeks of pregnancy. Most women who have morning sickness develop nausea and vomiting about one month after conception, but it may develop sooner in some women. Sometimes women report an increased in sensitivity to certain odors or smells that can sometimes cause nausea and/or vomiting.
Elevations in progesteron that occur early in pregnancy are thought to slow the emptying of the stomach and may be related to the development of nausea. Accompanying the characteristic "morning sickness" may be cravings for, or aversions to, specific foods or even smells. It is not unusual for a pregnant woman to change her dietary preferences, often having no desire to eat previous "favorite" foods. In most women, nausea and vomiting begin to subside by the second trimester of pregnancy.
Food cravings
Many women report cravings for certain foods during the early stages of pregnancy. These cravings can persist throughout the entire pregnancy.
Fatigue and tiredness
Fatigue and tiredness are symptoms experienced by many women in the early stages of pregnancy. Some women report feeling fatigued even in the weeks immediately prior to conception. The cause of this fatigue has not been fully determined, but it is believed to be related to rising levels of the hormone progesterone. Of course, fatigue is a very nonspecific symptom that can be related to many causes other than pregnancy.
Abdominal bloating
Some women may experience feelings of abdominal enlargement or bloating, but there is usually only a small amount of weight gain in the first trimester of pregnancy. In this early stage of pregnancy a weight gain of about one pound per month is typical. Sometimes women also experience mild abdominal cramping during the early weeks of pregnancy, which may be similar to the cramping that occurs prior to or during the menstrual period.
Frequent urination
A woman in the early stages of pregnancy may feel she has to urinate frequently, especially at nighttime, and she may leak urine with a cough, sneeze, or laugh. The increased desire to urinate may have both physical and hormonal causes. Once the embryo has implanted in the uterus, it begins to produce the hormone known as human chorionic gonadotrophin (hCG), which is believed to stimulate frequent urination. Another cause of frequent urination that develops later is the pressure exerted by the growing uterus on the bladder.
Elevated basal body temperature
A persistently elevated basal body temperature (the oral temperature measured first thing in the morning, before arising from bed) is another characteristic sign of early pregnancy. An elevation in the basal body temperature occurs shortly after ovulation and persists until the next menstrual period occurs. Persistence of the elevated basal body temperature beyond the time of the expected menstrual period is another sign of early pregnancy.
Changes in nipple color
Women may notice a deepening of the color of the area surrounding the nipple, called the areola and/or a dark line going down from the middle of the central abdomen area to the pubic area (known as the linea nigra). Some degree of darkening of the areola persists after pregnancy in many women, but the linea nigra typically disappears in the months following delivery of the baby.
Melasma (darkening of the skin)
Some women may develop a so-called "mask of pregnancy" in the first trimester, referring to a darkening of the skin on the forehead, bridge of the nose, upper lip, or cheeks. The darkened skin is typically present on both sides of the face. Doctors refer to this condition as melasma or chloasma, and it is more common in darker-skinned women than those with lighter skin. Melasma can also occur in some conditions other than pregnancy. Women who have a family history of melasma are at greater risk of developing this sign of pregnancy.
Mood swings and stress
Mood swings and stress are common symptoms reported by many women in the early stages of pregnancy. Many women in the early stages of pregnancy describe feelings of heightened emotions or even crying spells. The rapid changes in hormone levels are believed to cause these changes in mood. Pregnant women may also notice more rapid and drastic changes in their moods.
Headaches
Some women report suffering from headaches early on in their pregnancy, which may be related to corresponding changes in hormone levels.
Labels: Pregnancy
Visitor
Labels
- Carcinoma (2)
- Dysmenorrhoea (4)
- Endometriosis (4)
- Female Genital Infection (3)
- Fluor Albus (4)
- General (3)
- Genital Prolapse (4)
- Gynecology (8)
- Infectious Disease in Pregnancy (13)
- Infertility (10)
- Menopause (3)
- Menstrual Disorder (10)
- Myoma Uteri (3)
- Obstetrics (13)
- Pelvic Floor (4)
- Pelvic Inflamatory Disease (3)
- Physiology of Human Reproductive System (4)
- Pregnancy (2)
- Sexually Transmitted Disease (6)
- Uterine Bleeding (4)
Followers
Facebook Badge
Copyright © 2009 Complicated Girl. All Rights Reserved.