Information Site About Reproductive System
About Me
Blog Archive
-
▼
2009
(58)
-
▼
November
(20)
- HYSTERECTOMY – SURGICAL PROCEDURES
- HYSTERECTOMY
- MYOMECTOMY
- FIBROID
- GONORRHOEA INFECTION
- SALPINGITIS
- PELVIC INFLAMATORY DISEASE
- ENDOMETRIOSIS – Treatment Options
- ENDOMETRIOSIS – causes and risk factors
- ENDOMETRIOSIS
- ADENOMYOSIS
- HUMAN FERTILIZATION
- EARLY PREGNANCY SYMPTOMS
- MENOPAUSE and SEXUAL ISSUES
- CYTOLYTIC VAGINOSIS
- MENOPAUSE- hormone replacement therapy
- VULVOVAGINAL CANDIDIASIS
- TRICHOMONIASIS
- BACTERIAL VAGINOSIS
- MENOPAUSE
-
▼
November
(20)
Monday, November 30, 2009
Pelvic Inflammatory Disease – PID
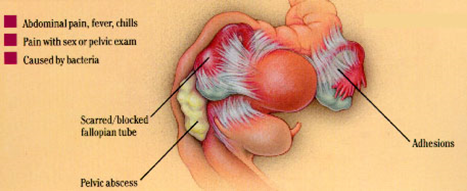
Pelvic inflammatory disease (PID) occurs when an infection spreads from the vagina to the cervix, endometrium (lining of the uterus) and fallopian tubes. The infection is usually sexually transmitted. It can also occur after a ruptured (burst) appendix or a bowel infection.
Some surgical procedures, such as abortion or insertion of an intrauterine device (IUD), can lead to PID.
The infection usually occurs in three stages - the cervix is infected first, followed by the endometrium and then the fallopian tubes.
The silent epidemic
PID is often called the ‘silent epidemic’ because it is common among sexually active women but does not always cause symptoms. About 10,000 women in Australia are treated for PID in hospital each year. About 10 to 30 times that number are treated as outpatients. Women aged 20 to 29 have the highest reported incidence of PID.
Signs and symptoms that can occur
Signs and symptoms of PID that may occur include:
- Lower abdominal pain or tenderness
- Menstrual disturbances
- Burning pain when urinating (dysuria)
- A change in smell, colour or amount of vaginal discharge
- Deep pain during sexual intercourse
- Fever.
Female infertility can be a devastating consequence
Scarring and blockage of the fallopian tubes is the most frequent long term complication of PID. Infertility occurs because the fertilised egg cannot pass through the tube to the uterus:
- One episode of PID doubles the risk of tubal infertility.
- The risk of fallopian tube blockage rises to 75 per cent after three or more episodes of PID.
- The risk of ectopic pregnancy (where the foetus develops outside the uterus) after one episode of PID is increased seven fold.
Chlamydia and gonorrhoea are the most common causes of PID
Chlamydia is responsible for 50 per cent of PID cases while gonorrhoea is the cause in 25 per cent of cases. The risk of fallopian tube blockage is slightly higher for PID caused by gonorrhoea. Both are bacterial infections and are sexually transmitted diseases (STDs). Non-specific urethritis, the most common STD among men, is most often caused by chlamydia.
Diagnosing PID
Your doctor will test for possible causes like chlamydia and gonorrhoea. In some cases, laparoscopy is required to correctly diagnose PID. Laparoscopy involves inserting an endoscope (which is like a surgical video camera) into the abdomen to view the reproductive organs.
Without treatment, chronic pain may develop
Chronic pain and, sometimes, severe disability can occur if PID is not treated. This is usually due to extensive scarring. Treatment involves:
- ANTIBIOTICS that are active against a broad range of organisms - amoxycillin (a type of penicillin) and doxycycline are usually prescribed.
- TESTING and TREATING male partners and treating them, if necessary - symptoms may be mild or non-existent in men.
- AVOIDING GENITAL SEXUAL XONTACT until the treatment is complete and a negative test result is obtained.
- SURGERY to remove scar tissue.
Protecting yourself from PID
To help prevent the transmission of the bacteria that can cause PID:
- Use condoms during vaginal or anal intercourse.
- Use condoms if you have an intrauterine device (IUD) inserted.
Use of the oral contraceptive pill may help
Sexually active women who are on the pill appear to have only one-third the risk of PID compared to women not on the pill. However, this data was collected in the 1970s and it is not known if the lower-dose pills more commonly used now have the same protective effect, although it is likely that they do.
Visitor
Labels
- Carcinoma (2)
- Dysmenorrhoea (4)
- Endometriosis (4)
- Female Genital Infection (3)
- Fluor Albus (4)
- General (3)
- Genital Prolapse (4)
- Gynecology (8)
- Infectious Disease in Pregnancy (13)
- Infertility (10)
- Menopause (3)
- Menstrual Disorder (10)
- Myoma Uteri (3)
- Obstetrics (13)
- Pelvic Floor (4)
- Pelvic Inflamatory Disease (3)
- Physiology of Human Reproductive System (4)
- Pregnancy (2)
- Sexually Transmitted Disease (6)
- Uterine Bleeding (4)
Followers
Facebook Badge
Copyright © 2009 Complicated Girl. All Rights Reserved.





0 comments:
Post a Comment