Information Site About Reproductive System
About Me
Blog Archive
-
▼
2009
(58)
-
▼
October
(21)
- IN VITRO FERTILIZATION - IVF
- OVULATION PAIN - MITTELSCHMERZ
- SPERM ANALYSIS
- INFERTILITY TREATMENT - MALE
- INFERTILITY - MALE
- DIAGNOSTIC METHODS IN FEMALE INFERTILITY
- POLYCYSTIC OVARIAN SYNDROME
- INFERTILITY -FEMALE
- PUBERTY
- HOW TO GET PREGNANT
- MIGRAIN and HORMONAL CHANGES
- IRREGULAR VAGINAL BLEEDING
- TOXIC SHOCK SYNDROME
- THERAPEUTIC OPTION PREMENSTRUAL SYNDROME
- PREMENSTRUAL SYNDROME
- OVULATION
- MENORRHAGIA
- DYSMENORRHOEA
- AMENORRHOEA
- MENSTRUAL CYCLE
- REPRODUCTIVE ORGAN SYSTEM
-
▼
October
(21)
Saturday, October 31, 2009
 In vitro fertilisation (IVF) is the process used to conceive a child outside the body. A woman’s eggs and a man’s sperm are placed together in a plastic dish for fertilisation. Once fertilised, the resulting embryos are placed back in the woman’s uterus in the hope that a successful pregnancy will follow.
In vitro fertilisation (IVF) is the process used to conceive a child outside the body. A woman’s eggs and a man’s sperm are placed together in a plastic dish for fertilisation. Once fertilised, the resulting embryos are placed back in the woman’s uterus in the hope that a successful pregnancy will follow.
The IVF procedure
IVF is not one simple procedure, but a series of steps over several weeks. The steps involved in this procedure are outlined below.
Stimulating the ovaries
Hormones are usually given to stimulate the ovaries to produce more than the usual one egg per cycle. This is to enable the collection of several eggs.The development of the eggs is monitored by one or two blood tests and ultrasounds. The ultrasound and blood tests ensure that eggs are collected at precisely the right time.
Collecting the eggs
 The ultrasound is inserted in the vagina and a very fine needle is threaded through a guide, which is attached to a probe. Only a light anaesthetic is required for this procedure. The ultrasound monitor shows where the follicles are. The needle pierces the follicle and extracts the follicular fluid, which contains the egg.
The ultrasound is inserted in the vagina and a very fine needle is threaded through a guide, which is attached to a probe. Only a light anaesthetic is required for this procedure. The ultrasound monitor shows where the follicles are. The needle pierces the follicle and extracts the follicular fluid, which contains the egg.
Fertilisation and embryo transfer
A couple of hours after egg collection, the man provides a sample of semen. In a standard IVF treatment, the eggs are mixed with the sperm in a culture dish. For intracytoplasmic sperm injection (ICSI) treatment, one sperm is injected directly into the cytoplasm of each egg.
If an egg is fertilised by a sperm, a zygote or pre-embryo will begin to develop. The pre-embryo remains in the incubator for one or two days, until it has divided into two or four cells. Following fertilisation, two to three embryos will be transferred to the uterus using a soft, fine catheter. This procedure (known as embryo transfer) is quite painless, similar to a smear test, and requires no anaesthetic.
For the gamete intrafallopian transfer (GIFT) program, eggs and sperm are placed directly into the fallopian tubes, allowing fertilisation to take place in the natural way. The procedure is performed using a laparoscope, and a general anaesthetic is required. This procedure is rarely used now.
Pregnacy test results
Two weeks after the transfer, a blood test is taken to determine if the woman is pregnant.
Possible risks and side effects
There is no clear evidence that infertility medicines, if properly used, increase the risk of birth defects or cancer. The increase in the hormone oestrogen can cause breast tenderness, slight nausea, dizziness and slight abdominal swelling. Occasionally, too many follicles develop and a condition called ovarian hyperstimulation syndrome (OHSS) may occur. This is an unpleasant experience, which may include marked abdominal swelling, nausea, vomiting and diarrhoea, lower abdominal pain and shortness of breath. There is also a theoretical risk (very rare) of damaging organs, or causing infection or bleeding, with the collection needle.
Things to remember
- IVF is a process where fertilisation of an egg occurs outside of the body.
- IVF is not one procedure but rather a series of steps taken over several weeks.
- While infertility drugs have some side effects, there is no evidence that they cause cancer or birth defects.
Labels: Infertility
 Ovulation is a phase of the female menstrual cycle, which involves the release of an egg (ovum) from one of the ovaries. For most women, ovulation occurs about once every month until menopause, apart from episodes of pregnancy and breastfeeding.
Ovulation is a phase of the female menstrual cycle, which involves the release of an egg (ovum) from one of the ovaries. For most women, ovulation occurs about once every month until menopause, apart from episodes of pregnancy and breastfeeding.
About one in five women experience pain and discomfort during ovulation. The duration of the pain varies from one woman to the next, but ranges from a few minutes to 48 hours. In most cases, ovulation pain doesn’t mean that anything is wrong. However, severe pain may sometimes be symptomatic of gynaecological conditions including endometriosis. See your doctor if your ovulation pain lasts longer than three days or is associated with other unusual menstrual symptoms, such as heavy bleeding. Ovulation pain is also known as mid-cycle pain and mittelschmerz (German for ‘middle pain’).
Symptoms
The symptoms of ovulation pain can include:
- Pain in the lower abdomen, just inside the hip bone.
- The pain typically occurs about two weeks before the menstrual period is due.
- The pain is felt on the right or left side, depending on which ovary is releasing an egg.
- The pain may switch from one side to the other from one cycle to the next, or remain on one side for a few cycles.
- The pain sensation varies between individuals - for example, it could feel like uncomfortable pressure, twinges, sharp pains or cramps.
- The duration of pain ranges anywhere from minutes to 48 hours.
The exact cause of ovulation pain is not clear, but theories include:
- Emerging follicle - hormones prompt the ovaries to produce around 20 follicles. Each follicle contains an immature egg (ovum) but only one follicle usually survives to maturity. It is supposed that ovulation pain is caused by the expanding follicle stretching the membrane of the ovary.
- Ruptured follicle - when the egg is mature, it bursts from the follicle. This may cause slight bleeding. The peritoneum (abdominal lining) could be irritated by the blood or fluids from the ruptured follicle, and this may trigger the pain.
In most cases, ovulation pain is harmless. However, severe and prolonged ovulation pain, or other pains felt in the lower abdomen, can be symptomatic of various medical conditions including:
- Salpingitis - inflammation of the fallopian tubes following an infection.
- Chronic pelvic inflammatory disease - inflammation following an infection.
- Endometriosis - the lining of the womb (endometrium) grows in other locations, such as the bowel. Other symptoms include painful periods and painful sex.
- Ovarian cyst - an abnormal pocket of fluid that develops on the ovary.
- Ectopic pregnancy - a pregnancy that develops outside of the womb, most commonly in one of the fallopian tubes. Symptoms include cramping, abdominal pain and vaginal bleeding. Seek urgent medical help.
- Appendicitis - inflammation of the appendix can sometimes be confused with ovulation pain. Seek urgent medical help if the pain is on the right side of your abdomen and you are experiencing nausea and vomiting.
- Other gastrointestinal problems - lower abdominal pain can be symptomatic of a range of gastrointestinal problems, including perforated ulcer, gastroenteritis and inflammatory bowel disease.
Tests that help determine whether ovulation pain is harmless or caused by infection or disease may include:
- Medical history
- Physical examination, including an internal pelvic examination
- Blood tests
- Cervical cultures
- Abdominal ultrasound
- Vaginal ultrasound
- Exploratory surgery (laparoscopy or ‘keyhole’ surgery).
Consult with your doctor to make sure that your ovulation pain isn’t caused by any underlying medical problem. Suggestions on taking care of benign ovulation pain yourself include:
- Relax. If the pain is particularly bothersome, rest in bed whenever you can.
- Use pain-killing medication.
- Warmth on the lower abdomen may help. Use heat packs, hot water bottles or warm baths.
- Take anti-inflammatory drugs. See your doctor or pharmacist for recommendations.
- The Pill and other forms of hormonal contraceptive can prevent ovulation pain because they stop ovulation. Talk over this option with your doctor.
- See your doctor if you experience ovulation pain that lasts longer than three days, or if you have other symptoms such as heavy bleeding or discharge.
Family planning
Chances of conception are high if a couple have sex in the days before, during and after ovulation. Some women rely on ovulation pain to help them plan a pregnancy. However, it is unwise to rely on ovulation pain alone if you’re trying to avoid pregnancy. Always use other methods of birth control.
Things to remember
- About one in five women experience pain during ovulation that can last from a few minutes to 48 hours.
- Ovulation pain is usually harmless, but can sometimes indicate various medical conditions such as endometriosis.
- See your doctor if your ovulation pain lasts longer than three days or is associated with other unusual menstrual symptoms, such as heavy bleeding.
Labels: Menstrual Disorder
Friday, October 30, 2009
Semen analysis
A semen analysis evaluates certain characteristics of a male's semen and the sperm contained in the semen. It may be done while investigating a couple's infertility or after a vasectomy to verify that the procedure was successful.
Relation to fertility
The characteristics measured by semen analysis are only some of the factors in semen quality. One source states that 30% of men with a normal semen analysis actually have abnormal sperm function.[1] Conversely, men with poor semen analysis results may go on to father children.[2][3]
Collection methods
The most common way to collect a semen sample is through masturbation, directing the sample into a clean cup.[2]
A sample may also be collected during intercourse in a special type of condom known as a collection condom. Collection condoms are made from silicone or polyurethane, as latex is somewhat harmful to sperm.[4] Many men prefer collection condoms to masturbation, and some religions prohibit masturbation entirely. Adherents of religions that prohibit contraception, such as Catholicism, may use collection condoms with holes pricked in them.[5]
A third option for collecting a sample is through coitus interruptus (withdrawal). With this technique, the man removes his penis from his partner near the end of intercourse and ejaculates into a cup.
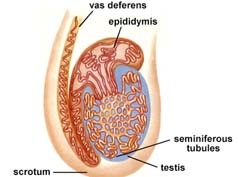
Finally, if a blockage in the vas deferens is suspected to impede fertility, semen can be taken directly from the epididymis. Such a collection is called per cutaneous epididymal sperm aspiration (PESA). Alternatively, the testicular tissue itself, instead of the sperm produced can be investigated. Then, the collecting method is called TESE.[6]
Tested characteristics
Examples of parameters measured in a semen analysis are: sperm count, motility, morphology, volume, fructose level and pH.
1. Sperm count
Approximate pregnancy rate varies with amount of sperm used in an artificial insemination cycle. Values are for intrauterine insemination, with sperm number in total sperm count, which may be approximately twice the total motile sperm count.
Sperm count, or sperm concentration to avoid mixup, measures the concentration of sperm in a man's ejaculate, distinguished from total sperm count, which is the sperm count multiplied with volume.[7] Anything over 20 million sperm per milliliter is considered normal.[1][2] Anything less is considered oligospermia. A vasectomy is considered successful if the sample is azoospermic. Some define success with rare non-motile sperm are observed (fewer than 100,000 per millilitre).[8] Others advocate obtaining a second semen analysis to verify the counts are not increasing (as can happen with re-canalization) and others still may perform a repeat vasectomy for this situation.
The average sperm count today is around 60 million per milliliter in the Western world, having decreased by 1-2% per year from a substantially higher number decades ago.[9]
2. Motility
The motility of the sperm is evaluated. WebMD defines normal motility as 60% of observed sperm, or at least 8 million per millilitre, showing good forward movement.[2] The World Health Organization has a similar value of 50% and this must be measured within 60 minutes of collection. A man can have a total number of sperm far over the limit of 20 million sperm cells per milliliter, but still have bad quality because too few of them are motile. However, if the sperm count is very high, then a motility of less than 60% might not matter, because the fraction might still be more than 8 million per millilitre. The other way around, a man can have a sperm count far less than 20 million sperm cells per millilitre and still have good motility, if more than 60% of those observed sperm cells show good forward movement.
A more specified measure is motility grade, where the motility of sperm are divided into four different grades:[10]
- Grade 4: Sperm with progressive motility. These are the strongest and swim fast in a straight line. Sometimes it is also denoted motility a.
- Grade 3: (non-linear motility): These also move forward but tend to travel in a curved or crooked motion. Sometimes also denoted motility b.
- Grade 2: These have non-progressive motility because they do not move forward despite the fact that they move their tails.
- Grade 1: These are immotile and fail to move at all.
3. Morphology
The morphology of the sperm is also evaluated. With WHO criteria as described in the old manual of 1989, a sample is normal if 30% or more of the observed sperm have normal morphology.[1] If morphology is evaluated using the Tygerberg strict criteria developed by Dr. Roelof Menkveld, Tygerberg Hospital, South Africa, and disseminated by Dr. Thinus Kruger from the same hospital,[11] a sample is normal if 14% or more of the observed sperm have normal morphology.[1]. The Tygerberg strict criteria for morpology assessment are recommended in the most recent WHO manual on semen analysis (WHO 1999). According to the above references, morphology was developed as a predictor of success in fertilizing oocytes during invitro fertilization.
4. Volume
The volume of the sample is measured. WebMD advises that volumes between 1.0 mL and 6.5 mL are normal;[2] WHO criteria specify that any volume greater than 2.0 mL is normal. Low volume may indicate partial or complete blockage of the seminal vesicles, or that the man was born without seminal vesicles.[1] In clinical practice, a volume of less than 2 mL in the setting of infertility and absent sperm should prompt an evaluation for obstructive azoospermia. A caveat to this is be sure it has been at least 48 hours since the last ejaculation to time of sample collection.
5. Fructose level
The level of fructose in the semen is measured. WebMD lists normal as at least 3 mg/mL.[2] WHO specifies a normal level of 13 μmol per sample. Absence of fructose may indicate a problem with the seminal vesicles.[1]
6. pH
The pH of the sample is measured. WebMD lists a normal range of 7.1-8.0;[2] WHO criteria specify normal as 7.2-7.8.[1] Acidic ejaculate (lower pH value) may indicate one or both of the seminal vesicles are blocked. A basic ejaculate (higher pH value) may indicate an infection.[1] A pH value outside of the normal range is harmful to sperm.[2]
7. Liquefaction
The liquefaction is the process when the gel formed by proteins from the seminal vesicles is broken up and the semen becomes more liquid. It normally takes less than 20 minutes for the sample to change from a thick gel into a liquid. An abnormally long liquefaction (more than 30 minutes at 37 24°C) time may indicate an infection.
8. MOT
MOT is a measure of how many million sperm cells per ml are highly motile[12], that is, approximately of grade 4, or sometimes also taking grade 3 into account. Thus, it is a combination of sperm count and motility.
With a straw volume of 0.5 milliliter per straw, the general guideline is that, for intracervical insemination (ICI), straws making a total of MOT40 is recommended. This is equal to 8 straws with MOT5, or 2 straws of MOT20. For intrauterine insemination (IUI), straws making a total of MOT10 is regarded sufficient.[13] In WHO terms, it is thus recommended to use approximately 20 million grade 3+4 sperm in ICI, and 5 million ones in IUI.
Total motile spermatozoa
Total motile spermatozoa (TMS)[14] or total motile sperm count (TMSC)[15] is a combination of sperm count, motility and volume, measuring how many million sperm cells in an entire ejaculate are motile.
Use of approximately 20 million grade 3+4 sperm in ICI, and 5 million ones in IUI may be an approximate recommendation.
9. Others
The sample is tested for white blood cells. A high level of white blood cells (over 1 million per milliliter) may indicate an infection.[1]
Abnormalities
- Aspermia: absence of semen
- Azoospermia: absence of sperm
- Oligospermia: low number of sperm
- Asthenozoospermia: poor sperm motility
- Teratozoospermia: sperm carry more morphological defects than usual
Factors that influence results
Compared to samples obtained from masturbation, semen samples from collection condoms have higher total sperm counts, sperm motility, and percentage of sperm with normal morphology. For this reason, they are believed to give more accurate results when used for semen analysis.[4]
How long the man has abstained prior to providing the sample for analysis affects the results. Longer periods of abstinence correlate with poorer results - one study found that men with repeated normal results produced abnormal samples if they abstained for more than 10 days. It is recommended not to abstain for more than one or two days before providing the semen sample for analysis.[16]
If the results from a man's first sample are subfertile, they must be verified with at least two more analyses. At least 2 to 4 weeks must be allowed between each analysis.[17] Results for a single man may have a large amount of natural variation over time, meaning a single sample may not be representative of a man's average semen characteristics.[18] In addition, sperm physiologist Joanna Ellington believes that the stress of producing an ejaculate sample for examination, often in an unfamiliar setting and without any lubrication (most lubricants are somewhat harmful to sperm), may explain why men's first samples often show poor results while later samples show normal results.[3]
A man may prefer to produce his sample at home rather than at the clinic. The site of semen collection does not affect the results of a semen analysis.[19]
Measurement methods
Volume can be determined by measuring the weight of the sample container, knowing the mass of the empty container. Sperm count and morphology can be calculated by microscopy. Sperm count can also be estimated by kits that measure the amount of a sperm-associated protein, and are suitable for home use. [20]
Computer Assisted Semen Analysis (CASA) is a catch-all phrase for automatic or semi-automatic semen analysis techniques. Most systems are based on image analysis, but alternative methods exist such as tracking cell movement on a digitizing tablet.[21][22] Computer-assisted techniques are most-often used for the assessment of sperm concentration and mobility characteristics, such as velocity and linear velocity. Although many systems can give very accurate information about motility patterns of motile sperm, immotile sperm cannot accurately be distinguished from other cells, particles or debris without addition of staining. The first CASA systems in general cannot give reliable results for sperm concentration and proportions of sperm with different grades of motility, at least not in semen samples, where there are many other particles, cells and debris. Even when it comes to motility, most systems cannot give reliable results when the concentration of motile sperm leads to significant "crossed paths" - due to difficulties to decide if there were two sperm crossing each others way, or if there were for instance four sperm moving close to each other. Nowadays, there are CASA systems, based on image analysis and using new techniques, with near perfect results, and doing full analysis in a few seconds.
CASA Systems
SQA-V - The SQA-V, also known as the 'Sperm Quality Analyzer or Spermalite, is a high performance sperm analysis instrument used to test male fertility. It combines electro-optics, computer algorithms and video microscopy to provide a precise and accurate 75 second automated semen analysis. This device is manufactured by Medical Electronic Systems [23], who specializes in rapid, automated semen analysis. The main reason the SQA-V is a growing instrument among the semen analysis community is due to the speed, accuracy, and precision to run a semen sample. In addition, the SQA-V semen analysis eliminates inter-operator variables from the manual method, and still provides 16 clinical parameters including: Sperm Concentration, Rapid Progressive motility, Slow Progressive motility, Non-progressive motility, Immotility, %Normal Morphology, and more.
A study was conducted by the world renowned Cleveland Clinic comparing the SQA-V to the Manual method and the CASA device, presenting results favoring the SQA-V. [24]
ISAS - Integrated Semen Analysis System is a CASA system based on image analysis from the company Projects i Serveis R+D S.L., also known as PROISER. PROISER was founded on 2004 by a team of CASA developers (SCA 96, SCA 98 and SCA 2002) with more than 15 years in experience of seminal analysis by computer image analysis. ISAS can be considered as the most complete and easiest-to-use system in market which, furthermore, works in different hardware and operating-system conditions, in order to adapt as much as possible to the needs of our users. Current computers and AAVT technology allows a very good matching of spermatozoon, thanks to the tail and morphology analysis made at the same time as motility analysis. Only motility and concentration analysis give to the customers more tan 17 sperm parameters, but also ISAS analyzes automatically stained morphometry, giving 15 parameters and DNA fragmentation analysis. ISAS has been developed to be used in several species, from classical species like human, boar or bull to new research species like cod or some small rodents. There are a lot of publications and works in progress with ISAS like [25]. A list of last publications with this CASA system can be found on publications with ISAS
Sperm Class Analyzer - The Sperm Class Analyzer, also known as 'SCA' from the company Microptic S.L., provides fast, accurate and objectively repeatable results. This would be impossible to attain using traditional (subjective) methods. This CASA system has the following modules: SCA Motility & Concentration: The system provides immediately and objectively detailed results of motility and concentration in a complete report. SCA Morphology: Following a manual or automatic image capture, a precise morphological and morphometric analysis of each spermatozoid is provided in real time. SCA DNA Fragmentation: Analysis of halo formation of the samples prepared for study of the DNA fragmentation provides detailed numerical data for each of the cells. SCA Vitality: Automatically analyze the vitality of a sperm sample. All this modules can be used with a motorized stage or link the database with any hospital system.
IVOS Sperm Analyzer - The Integrated Visual Optical System (IVOS) was developed by Hamilton Thorne, the leading manufacturer of CASA systems since 1986. The IVOS is found in hospitals, universities, IVF clinics, pharmaceutical companies, contract labs, reproductive toxicology labs, veterinary clinics and animal breeding facilities around the world. The standard IVOS software may be used to analyze sperm of multiple species, with a specific program geared toward analysis of rat sperm. The IVOS is unique in that it is the only CASA system that integrates the optical system within the unit, so that an external microscope is not needed. The light source of the IVOS produces stroboscopic illumination to provide blur free sperm images. This stroboscopic light source is especially beneficial when utilizing the IDENT fluorescent option on the IVOS as it allows the analysis of motile sperm under fluorescent illumination without adverse affect on sperm motility or velocity (this is not possible with continuous light fluorescent microscopes). Analysis using the IVOS IDENT provides highest accuracy of sperm counts in samples with a high degree of detritus, such as occurs in egg yolk extended samples or naturally in some species, such as rabbits. Samples are placed on a computer-controlled, heated stage which maintains samples at the proper analysis temperature and automatically moves to selected fields for analysis. A field of sperm are analyzed in just 0.5 second with a level of accuracy and repeatability unobtainable by visual assessment. Results calculated include count, concentration, motility, progressive motility, curvilinear velocity (VCL), straight line velocity (VSL), average path velocity (VAP), linearity (LIN), straightness (STR), amplitude of lateral head displacement (ALH) and beat cross frequency (BCF). Custom software packages are available, such as Animal Breeder, Equine Breeder and Animal Motility, which provide additional features specific to the target industries. In addition, the TOX IVOS is a complete system configured specifically for the inticacies of rat sperm analysis. Two automated morphology options, Dimesnisons Strict Morphology (developed and validated by Dr. Thinus Kruger) and Metrix user defined morphology are available. Another fluorescent option is VIADENT, which permits the analysis of motility and viability on the same live sample.
"Our results suggest that the VIADENT option of the IVOS system is capable of a rapid, accurate and objective evaluation of both viability and motility parameters using large numbers of spermatozoa. Application of this technique in the industry may prove useful in the clinical assessment of fertilizing potential of equine spermatozoa." [26]
CEROS Sperm Analyzer - Also from Hamilton Thorne and built upon the same analysis algorithms and software interface as the IVOS, the CEROS offers the same level of accuracy and reliability for sperm analysis. The CEROS uses an external negative phase contrast microscope for image visulaization and analysis. The system comes complete with motility analysis software, microscope, camera, computer and monitor. The CEROS is also compatible with both the Dimensions and Metrix morphology options and can be used for to analyze sperm from all species except rat. Both systems offer 4 levels of quality control as well as high-level security and audit trail for data inetgrity. A searacble list of publications featuring the Hamilton Thorne IVOS and CEROS CASA systems is found on Connotea.
References
- "Understanding Semen Analysis". Stonybrook, State University of New York. 1999. http://www.uhmc.sunysb.edu/urology/male_infertility/SEMEN_ANALYSIS.html. Retrieved 2007-08-05.
- Essig, Maria G.; Edited by Susan Van Houten and Tracy Landauer, Reviewed by Martin Gabica and Avery L. Seifert (2007-02-20). "Semen Analysis". Healthwise. WebMD. http://www.webmd.com/infertility-and-reproduction/guide/semen-analysis?page=1. Retrieved 2007-08-05.
- Ellington, Joanna (2004). "Understanding a Sperm Analysis". INGfertility. http://www.preseed.com/FAQs/FAQ4.php. Retrieved 2008-06-28.
- Dr. Joanna Ellington (January 2005). Use of a Specialized Condom to Collect Sperm Samples for Fertility Procedures. INGfertility. http://www.preseed.com/FAQs/FAQ4.php#Using_a_Sperm_Collection_Condom. Retrieved 2008-06-28.
- Kippley, John; Sheila Kippley (1996). The Art of Natural Family Planning (4th addition ed.). Cincinnati, OH: The Couple to Couple League. pp. pp.306–307. ISBN 0-926412-13-2.
- Fertility Center, Stockholm (translated from Swedish)
- sharedjourney.com - Male Infertility Testing
- Rajmil O, Fernández M, Rojas-Cruz C, Sevilla C, Musquera M, Ruiz-Castañe E (2007). "Azoospermia should not be given as the result of vasectomy" (in Spanish; Castilian). Arch. Esp. Urol. 60 (1): 55–8. PMID 17408173.
Dhar NB, Bhatt A, Jones JS (2006). "Determining the success of vasectomy". BJU Int. 97 (4): 773–6. doi:10.1111/j.1464-410X.2006.06107.x. PMID 16536771. - The sperm count has been decreasing steadily for many years in Western industrialized countries: Is there an endocrine basis for this decrease? The Internet Journal of Urology TM. ISSN: 1528-8390
- Shared Journey: Semen Analysis
- "Semen analysis morphology". IVF 1. 2005-10-27. http://www.ivf1.com/Semen-analysis-morphology/. Retrieved 2007-08-05.
- Cryos FAQs - What does MOT mean?
- Cryos FAQs - What is the recommended quantity and quality by ordering of donor semen?
- Merviel P, Heraud MH, Grenier N, Lourdel E, Sanguinet P, Copin H (November 2008). "Predictive factors for pregnancy after intrauterine insemination (IUI): An analysis of 1038 cycles and a review of the literature". Fertil. Steril.. doi:10.1016/j.fertnstert.2008.09.058. PMID 18996517.
- Pasqualotto EB, Daitch JA, Hendin BN, et al. (October 1999). "Relationship of total motile sperm count and percentage motile sperm to successful pregnancy rates following intrauterine insemination". J. Assist. Reprod. Genet. 16 (9): 476–82. doi:10.1023/A:1020598916080. PMID 10530401. http://www.kluweronline.com/art.pdf?issn=1058-0468&volume=16&page=476.
- Ellington, Joanna (2005). "How Long to Abstain for a Sperm Test/Analysis". INGfertility. http://preseed.com/FAQs/FAQ1.php#How_Long_to_Abstain_for_a_Sperm_Test/Analysis__. Retrieved 2008-06-28. , which cites:
- Levitas E, Lunenfeld E, Weiss N, et al. (June 2005). "Relationship between the duration of sexual abstinence and semen quality: analysis of 9,489 semen samples". Fertil. Steril. 83 (6): 1680–6. doi:10.1016/j.fertnstert.2004.12.045. PMID 15950636.
- Jurema MW, Vieira AD, Bankowski B, et al. (September 2005). "Effect of ejaculatory abstinence period on the pregnancy rate after intrauterine insemination". Fertil. Steril. 84 (3): 678–81. doi:10.1016/j.fertnstert.2005.03.044. PMID 16169402.
- Weschler, Toni (2002). Taking Charge of Your Fertility (Revised ed.). New York: HarperCollins. pp. p.189. ISBN 0-06-093764-5.
- "Adequate Analysis Frequency". Kokopelli Technologies. 2007. http://www.fertilityformen.com/info_why.php#frequency. Retrieved 2007-08-11.
- Shetty Licht R, Handel L, Sigman M (2007). "Site of semen collection and its effect on semen analysis parameters". Fertil Steril. 89: 395. doi:10.1016/j.fertnstert.2007.02.033. PMID 17482174.
- dailyprogress.com > Charlottesville company sends out its home male sterility tests By Brian McNeill. Published: May 14, 2009
- Mortimer ST (01 Jul 2000). "CASA--practical aspects". J. Androl. 21 (4): 515–24. PMID 10901437. http://www.andrologyjournal.org/cgi/reprint/21/4/515. Retrieved 2007-08-05.
- Hinting A, Schoonjans F, Comhaire F (1988). "Validation of a single-step procedure for the objective assessment of sperm motility characteristics". Int. J. Androl. 11 (4): 277–87. doi:10.1111/j.1365-2605.1988.tb01001.x. PMID 3170018.
- http://mes-ltd.com/overview.asp
- Agarwal A, Sharma R (2007). "Automation is the key to standardized semen analysis using the automated SQA-V sperm quality analyzer". Fertility and Sterility 87 (No. 1): 156. doi:10.1016/j.fertnstert.2006.05.083. http://www.clevelandclinic.org/ReproductiveResearchCenter/docs/agradoc230.pdf.
- L. Ramió, M.M. Rivera, A. Ramírez, I.I. Concha, A. Peña, T. Rigau and J.E. Rodríguez-Gil (2008). "Dynamics of motile-sperm subpopulation structure in boar ejaculates subjected to in vitro capacitation and further in vitro acrosome reaction". Theriogenology 69 (No. 4): 501. doi:10.1016/j.theriogenology.2007.10.021. http://www.sciencedirect.com/science?_ob=ArticleURL&_udi=B6TCM-4RCNPPD-1&_user=10&_coverDate=03%2F01%2F2008&_rdoc=15&_fmt=summary&_orig=browse&_srch=doc-info(%23toc%235174%232008%23999309995%23679613%23FLA%23display%23Volume)&_cdi=5174&_sort=d&_docanchor=&_ct=17&_acct=C000050221&_version=1&_urlVersion=0&_userid=10&md5=9926ba71bee609b30a7c56f73857f511.
- Wessel MT, Althouse GC. Validation of an objective approach for simultaneous assessment of viability and motility of fresh and cooled equine spermatozoa. Proceedings of the International Symposium on Equine Reproduction, Animal Reproduction Science 94 (2006) 21-22
Labels: Infertility
Approximately one in five couples have trouble conceiving a child. If a couple is unable to conceive after one year of unprotected intercourse, they are said to be subfertile. Around 40 per cent of fertility problems originate in the man, with causes including sperm abnormalities and blockages within structures of the reproductive system, such as the vas deferens. Many men have sufficient sperm to fertilise their partner's eggs in a test tube, even if they are unable to do so during sexual intercourse. In most cases, the couple can be helped with assisted reproductive technologies. For around one in 10 couples investigated for infertility, no cause is found. This is known as 'idiopathic infertility'.
Diagnosis methods
Investigating suspected infertility requires a range of tests for both the man and his partner. Some of the tests the man may undergo include:
- Physical examination - including medical history.
- Ultrasound scans - to check the health of reproductive organs.
- Blood tests - to check sex hormone levels.
- Semen analysis - a sperm sample is checked for abnormalities and antibodies.
- Testicular biopsy - the fine network of tubes within the testicles is checked for the presence of sperm.
Some of the reproductive technologies available to infertile men include:
- Surgery
- Hormone therapy
- Artificial insemination
- In vitro fertilisation (IVF)
- Intra cytoplasmic sperm injection (ICSI).
Surgery
Fertility may be impaired by varicocele, or the bloating of veins inside the testes. This condition can be surgically treated. The tubes within the male reproductive system that transport sperm may be blocked, perhaps by injury or vasectomy. In some cases, the blockage can be surgically removed or the tubes repaired. If this doesn't work, the man may undergo another surgical procedure called percutaneous epididymal sperm aspiration (PESA). Under local anaesthetic, a slender needle is inserted into the epididymis, which is the tube at the back of the testicle that collects and stores sperm. Sperm is removed, and either used immediately for IVF or frozen.
Hormone therapy
The pituitary gland in the brain releases the hormone gonadotropin, which prompts the testicles to produce sperm. In a small number of cases, male infertility is caused by insufficient levels of gonadotropin. Taking a synthesised version of this hormone can boost sperm production.
Artificial insemination
The man's semen is collected, washed and concentrated, then introduced (via instruments) into his partner's vagina, cervix, uterus or fallopian tubes, depending on the circumstances. This option is often chosen if the husband has functional problems (such as impotence), or if his sperm can't make it through the cervix to the uterus. Some of the factors that can stall sperm at the entrance to the uterus include:
- The man's seminal fluid contains antibodies that destroy his sperm
- The cervical mucus contains antibodies that destroy his sperm
- The cervical mucus is so acidic that sperm are unable to survive.
In vitro fertilisation (IVF)
In vitro fertilisation (IVF) is conception within a test tube (or similar). The woman undergoes ovulation induction (hormonal stimulation of her ovaries) and a number of eggs are removed. This is done through the vagina under ultrasound control. The collected eggs are then mixed with sperm previously collected from the woman's partner, and placed in a special incubator. The fertilised eggs are then implanted into the woman's uterus via a thin tube inserted through the cervix.
Intra cytoplasmic sperm injection (ICSI) Sometimes, semen contains too few sperm to make fertilisation possible through IVF. In this case, intra cytoplasmic sperm injection (ICSI) can be used. The eggs are removed from the woman's ovaries, then individually injected with a single sperm each. When the eggs are fertilised, the embryos are transferred into the uterus.
Sometimes, semen contains too few sperm to make fertilisation possible through IVF. In this case, intra cytoplasmic sperm injection (ICSI) can be used. The eggs are removed from the woman's ovaries, then individually injected with a single sperm each. When the eggs are fertilised, the embryos are transferred into the uterus.


Figure 1:
Immobilizing the sperm's tail before picking it up.

Figure 2:
Injection of sperm into the egg.

Figure 3:
Fertilized egg demonstrating the two nuclei – one from the father, one from the mother.
Pregnancy isn't always possible
Despite the sophistication of assisted reproductive technologies, pregnancy doesn't always happen. It depends on a range of factors, including the type of technology used and the reasons for the man's infertility. It should be remembered that assisted reproductive technologies can't improve the quality of sperm. Azoospermia, for example, means that the man's semen doesn't contain any sperm at all. In such cases, donor insemination may be considered. This involves artificially inseminating the partner with sperm from an anonymous donor.
Things to remember
- Around 40 per cent of fertility problems originate in the man, with causes including sperm abnormalities and blockages within structures of the reproductive system, such as the vas deferens.
- Some of the reproductive technologies available to infertile men include surgery to clear blockages, hormone therapy, artificial insemination, in vitro fertilisation (IVF) and intra cytoplasmic sperm injection (ICSI).
Labels: Infertility
New life begins when an egg from a woman is fertilised by sperm from a man. Around 20 million sperm per millilitre (ml) need to be present in the ejaculate, with enough mobility and strength to swim the journey to the fallopian tube, where conception normally takes place. The odds of a young fertile couple conceiving by having sexual intercourse around the time of ovulation are approximately one in five every month. A couple isn’t suspected of fertility problems until they have tried, and failed, to conceive for one year. Approximately 20 per cent of couples experience difficulties. In most cases, the couple can be helped with assisted reproductive technologies. Around 40 per cent of fertility problems originate in the man. Male fertility problems include poor quality sperm or blockages in the tubes of the reproductive system.
Obstructions
Sperm are made in the testicles. During ejaculation, sperm are pushed (by muscular contractions) through a series of small tubes called the epididymis, and mixed with seminal fluid from structures called seminal vesicles. The prostate gland also adds fluid. The semen is forced along a larger tube (vas deferens), into the urethra and out of the penis. In around one in three cases of male infertility, blockages or absences of tubes (including the vas deferens) are the cause of infertility. Causes may include vasectomy and injury.
Problems with sperm
 Problems with sperm numbers or quality are thought to be caused by genetic factors. Researchers have discovered that tiny fragments of the male chromosome may be missing in some men with sperm problems. This may cause:
Problems with sperm numbers or quality are thought to be caused by genetic factors. Researchers have discovered that tiny fragments of the male chromosome may be missing in some men with sperm problems. This may cause:
- Absent sperm (azoospermia) - the semen doesn’t contain any sperm. This may be caused by a blockage of the tubes, or testicular failure.
- Low sperm count (oligospermia) - the ejaculate has insufficient numbers of sperm to bring about conception.
- Abnormal shape - a healthy sperm is shaped like a streamlined tadpole. Abnormally shaped sperm may have problems penetrating the surface of the woman’s egg.
- Poor motility - a healthy sperm has a lashing tail, which helps it to swim through the woman’s reproductive system. Sperm with poor motility may swim feebly, or not at all.
Functional problems that can cause or contribute to male infertility include:
- Impotence - the inability to get or maintain an erection sufficient for sexual intercourse.
- Problems with the testicles - caused by injury, infection or chemotherapy.
- Prostatectomy - side effects of the surgical removal of the prostate gland, including infertility, impotence and incontinence.
- Certain disorders - such as multiple sclerosis or diabetes can cause erection and ejaculation difficulties.
- Antibodies - the man’s immune system makes antibodies that hinder the activity of sperm, such as reducing the sperm’s ability to latch onto the partner’s egg.
Hormonal problems
The levels of male sex hormones are regulated by a series of glands and their hormones. The pituitary gland in the brain influences hormone production in the testicles, under the guidance of another brain structure - the hypothalamus. A relatively uncommon cause of male infertility is the failure to make enough of the hormone gonadotrophin.
Idiopathic infertility
For around one in 10 couples investigated for infertility, no cause is found. This is called ‘unexplained’ or ‘idiopathic’ infertility.
Diagnosis methods
Investigating suspected infertility requires a number of tests for both the man and his partner. Diagnosing male infertility may involve:
- Semen analysis - a sample of the man’s semen is investigated in the laboratory and checked for abnormalities and the presence of antibodies.
- Blood tests - to assess hormone levels.
- Testicular biopsy - a fine needle and microscope are used to check the network of tubes to see if there are any sperm in them.
- Ultrasound test - to take pictures of the reproductive organs, such as the prostate gland.
There are no treatments available that can improve the quality of a man’s sperm. However, techniques can increase the odds of conception using the existing sperm quality. Treatment depends on the cause, but may include:
- Hormone therapy - if low sperm count is due to insufficient levels of the hormone gonadotrophin.
- Artificial insemination - the semen is collected and concentrated, then delivered with instruments directly into the partner’s uterus.
- In vitro fertilisation - conception occurs in the laboratory and the fertilised egg is implanted in the prepared uterus.
- Around 40 per cent of fertility problems originate in the man.
- Male fertility problems include poor quality sperm, low sperm count or blockages in the tubes of the reproductive system.
- Treatment options for poor sperm quality include artificially inseminating the partner with a concentrated sample of the man’s semen.
Labels: Infertility
Tuesday, October 27, 2009
Introduction
Any case of female infertility requires a careful and systematic anamnesis, which includes several questions that are generally not asked in the interview of most patients seen in a gynecological practice. It is after this important step that the necessary clinical investigations for the work-up of each given case can be selected in an appropriate manner in order to establish the correct diagnosis as precisely as possible and in the shortest length of time.
The three main questions to be answered are:
- Is the patient ovulating ?
- Are the conditions for implantation adequate ?
- Is the morphology of the uterus and the tubes normal ?
The answers are provided by the following methods:
Clinical evidence of ovulation
- Basal body temperature.
- Observation of the cervical mucus.
- Exfoliative vaginal cytology.
- Transvaginal sonography (ovarian follicles).
- Pituitary and ovarian hormones assays.
- Laparoscopy and direct observation of the ovaries.
Clinical evidence of readiness for uterine implantation
- Basal body temperature.
- Transvaginal sonography (thickness of the endometrium).
- Plasma progesterone assay.
- Endometrial biopsy.
- Hysteroscopy.
Clinical evidence of normality of the internal genital tract
- Hysterosalpingography.
- Transvaginal sonography.
- Hysteroscopy.
- Laparoscopy.
Clinical evidence of ovulation
Basal body temperature (BBT)
The early morning rectal temperature will rise approximately 0.5 to 0.7°C after ovulation and stay in a " plateau " for 12 to 14 days. This rise in BBT is due to a central effect of progesterone secretion. A slight drop of BBT might be observed 24 to 48 hours before ovulation, related to the estrogen peak secreted by the mature follicle.
Observation of the cervical mucus
Under the influence of the highest level of estrogen secretion from the dominant ovarian follicle, which precedes the ovulation, one can observe an abundant, clear and fluid secretion of mucus from the cervical canal. This transient secretion slightly but obviously dilates the external cervical os. It precedes ovulation by 4 to 2 days and is greatest on the day before ovulation. This mucus is highly receptive for the sperm penetration during sexual intercourse.
The cervical mucus disappears promptly after ovulation under the influence of progesterone secretion.
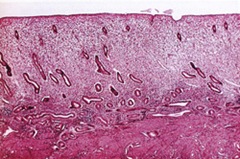
Exfoliative vaginal cytology
A vaginal smear, scraped from a lateral vaginal wall with an Ayres spatula or a wet cotton swab, provides a typical result at the time of ovulation, when examined under light microscope observation, after it has been stained with Papanicolaou or Schorr staining, or with any quick dye.
The superficial cells of the vaginal mucosa are flat, well scattered, with pyknotic nuclei and highly eosinophilic. As soon as ovulation has taken place, the cells become coiled, packed together and mostly basophilic .
Transvaginal sonography
The sonographic picture of a preovulatory follicle is well documented and typical. The mature follicle measures from 18 to 23 mm in average inner dimension.

After ovulation, the follicular wall becomes irregular and the fresh corpus luteum usually appears as a hypoechogenic structure and may contain some echoes corresponding to internal bleeding. The wall of the corpus luteum becomes thickened as the luteinization progresses .
Pituitary and ovarian hormone assays
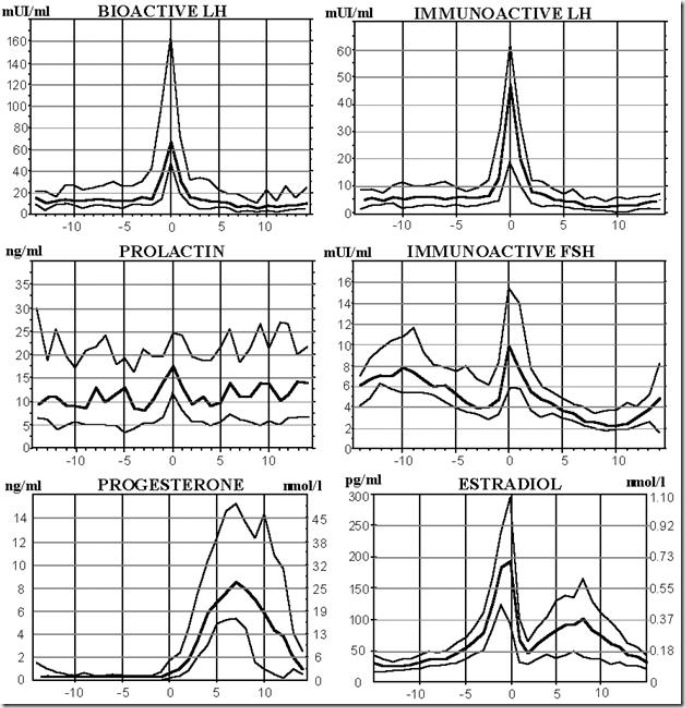
The secretion of LH can be detected daily in urine samples by radioimmunoassay. The LH peak usually precedes ovulation by 48 to 24 hours. At the same time, the secretion of estrogen produced by the dominant follicle, reaches a maximum in the peripheral venous blood. Soon after ovulation, the level of progesterone in the peripheral blood rises from 2.5 to 4.0 ng/ml and reaches its maximum from day 5 to day 10 after the LH peak, with a variation from 7 to 12 ng/ml. This intermediate luteal phase is the physiological time for uterine nidation .
A schematic representation of the hormonal secretory patterns throughout the menstrual cycle is illustrated below
Laparoscopy
A mature follicle increases ovarian size considerably and looks like a round bluish cyst with one or two capillaries seen on its surface.
After ovulation, the stigma of the follicular rupture can be easily recognized as a small hole surrounded by an hemorrhagic structure on the surface of the ovary. Scars of previous ovulations can also be recognized on the surface of both ovaries. Clear yellowish follicular fluid can be found in the pouch of Douglas.
Clinical evidence of readiness for uterine implantation
Basal body temperature
A sustained " plateau " of 12 to 14 days following ovulation, is indicative of a good progesterone secretion from the corpus luteum, at least of 4 ng/ml in the peripheral blood.
Transvaginal sonography
The thickness of the secretory endometrium can be precisely measured. At its thickest, it reaches 8 to 14 mm, including both layers, and should be echogenic in a regular manner.
Plasma progesterone assays
In order to have a good evaluation of the secretion of the corpus luteum, one should obtain at least three to four blood samples, for instance every other day, starting from the third postovulatory day.
Endometrial biopsy
The tissue sample should be aspired either with a Novak cannula or with a plastic Cornier’s Pipelle around the time when nidation normally takes place, which means between day 20 to 22 of the cycle. Dating of the endometrial biopsy requires strict histological criteria (6).
Hysteroscopy
Using a small hysteroscope of 5 mm or 3 mm of diameter, an hysteroscopic examination of the uterine cavity can be easily performed on an out-patient basis in a clinic or in the office, with or without anesthesia. The examination can rule out the presence of uterine polyps, synechiae, or endometritis, all of which could interfere with nidation (5,15).
Clinical evidence of normality of the internal genital tract
Hysterosalpingography
As in the case of other medical methods of investigation, strict technique is necessary in order to obtain precise information. A perfectly frontal view and also a good lateral view of the uterus, with a position of the uterus body being strictly parallel to the radiological film, is necessary to appreciate the size, the morphology and the outline of the uterine cavity.
A lateral view of a correct exposure of both tubes gives more information on their morphology than the frontal view. Also, the lateral view gives a better picture of the isthmic segment of the uterus and of its width in case of a suspected incompetence of the internal cervical os.
Until fibroscopic tools have been utilized enough and a sufficient optical knowledge on the inside morphology of the fallopian tubes has been accumulated, hysterosalpingography remains the only way to investigate the intramural segment and the isthmic segment of the fallopian tubes.
Pelvic adhesions can only be demonstrated by this radiological method, if a sufficient amount of opaque medium has been spread into the pelvis or, better, if a complementary hydrotubation with sterile saline is used at the end of the procedure, and if the last picture is taken after the patient has been leaned alternately on each side for a few minutes (" brassage ") .
Transvaginal sonography
With the use of a vaginal sound, we can now easily measure the size of the uterus, and observe the structure of the endometrium and of the myometrium. Polyps, myomas, internal synechiae and congenital malformations are well documented in specialized text books. Ovarian cysts and sactosalpinx can also be easily recognized with transvaginal sonography.
Hysteroscopy
With this method, using either CO2 gas or saline solution as a dilatation medium, the entire uterine cavity can be explored, and pathological findings detected, even those which can be sometimes missed with the hysterosalpingography.
The openings of the fallopian tubes in the uterine cavity can also be observed and demonstrated to be free of any obstacle as polyp or fibrotic tissue .
Laparoscopy
Trans- or paraumbilical laparoscopy remains the most complete method to explore the anatomical situation of both fallopian tubes and their relation with the adjacent ovaries. By means of direct optical observation, one can detect unsuspected peritubal and periovarian adhesions, or asymptomatic endometriosis, or agglutination of the fimbriae of the distal portion of the tubes.
With the advent of fine fibrotic catheters, introduced into the open fallopian tubes under laparoscopic control, we should be able to examine the internal appearance of the ampullary segments and detect small internal adhesions or post-inflammatory atrophy of the tubal epithelia .
References
- Bianchi, P.G., Rivest, R., Bischof, P., and Campana A. (1992): Bioactive-LH in the assessment of normal cycle phases. Abstracts from the 8th meeting of the European Society of Human Reproduction and Embriology. Hum. Reprod., A. 40, p. 28.
- Fleischer, A.C., and Kepple, S.M. (1992): Transvaginal Sonography. A Clinical Atlas. Pippincott Co., Philadelphia.
- Givens, J.R. (1978): Endocrine Causes of Menstrual Disorders. Year Book Medical Publishers Inc., Chicago.
- Gomel, V., Taylor, P.J., Yuzpe, A.A., and Rioux, J.E.: Laparoscopy and Hysteroscopy in Gynecologic Practice. Year Book Medical Publishers Inc., Chicago.
- Koss, L.G. (1992): Diagnostic and its Histopathologic Bases, 4th ed. J.P. Lippincott Co., Philadelphia.
- Rozin, S. (1965): Uterosalpingography in Gynecology. Thomas, Springfield.
- Siegler, A.M. (1967): Hysterosalpingography. Harper & Row, New York.
- Speroff, L., Glass, R.H., and Kase, N.G. (1983): Clinical Gynecologic Endocrinology and Infertility, 3rd ed. Williams and Wilkins, Baltimore.
- Tristant, H., and Benmussa, M. (1981): Atlas d’hystérosalpingographie, 2nd ed. Masson, Paris.
- Van der Pas, H., Van Herendael, B., Van Lith, D., and Keith, L. (1983): Hysteroscopy. MTP Press Limited, Boston.
- Wied, G.L., and Bibbo M. (1975): In: Gynecologic Endocrinology, edited by J.J. Gold. P.B. Hoeber, New York.
Labels: Infertility
Monday, October 26, 2009
 Polycystic (pah-lee-SIS-tik) ovary syndrome (PCOS) is a health problem that can affect a woman's menstrual cycle, ability to have children, hormones, heart, blood vessels, and appearance. With PCOS, women typically have:
Polycystic (pah-lee-SIS-tik) ovary syndrome (PCOS) is a health problem that can affect a woman's menstrual cycle, ability to have children, hormones, heart, blood vessels, and appearance. With PCOS, women typically have:
- high levels of androgens (AN-druh-junz). These are sometimes called male hormones, although females also make them.
- missed or irregular periods
- many small cysts (sists) in their ovaries. Cysts are fluid-filled sacs.
How many women have polycystic ovary syndrome (PCOS)?
About one in ten women of childbearing age has PCOS. It can occur in girls as young as 11 years old. PCOS is the most common cause of female infertility (not being able to get pregnant).
What causes polycystic ovary syndrome (PCOS)?
The cause of PCOS is unknown. Most researchers think that more than one factor could play a role in developing PCOS. Genes are thought to be one factor. Women with PCOS tend to have a mother or sister with PCOS. Researchers also think insulin could be linked to PCOS. Insulin is a hormone that controls the change of sugar, starches, and other food into energy for the body to use or store. For many women with PCOS, their bodies have problems using insulin so that too much insulin is in the body. Excess insulin appears to increase production of androgen. This hormone is made in fat cells, the ovaries, and the adrenal gland. Levels of androgen that are higher than normal can lead to acne, excessive hair growth, weight gain, and problems with ovulation.
Does polycystic ovary syndrome (PCOS) run in families?
Most researchers think that PCOS runs in families. Women with PCOS tend to have a mother or sister with PCOS. Still, there is no proof that PCOS is inherited.
What are the symptoms of polycystic ovary syndrome (PCOS)?
Not all women with PCOS share the same symptoms. These are some of the symptoms of PCOS:
- infrequent menstrual periods, no menstrual periods, and/or irregular bleeding
- infertility (not able to get pregnant) because of not ovulating
- increased hair growth on the face, chest, stomach, back, thumbs, or toes—a condition called hirsutism (HER-suh-tiz-um)
- ovarian cysts
- acne, oily skin, or dandruff
- weight gain or obesity, usually carrying extra weight around the waist
- insulin resistance or type 2 diabetes
- high cholesterol
- high blood pressure
- male-pattern baldness or thinning hair
- patches of thickened and dark brown or black skin on the neck, arms, breasts, or thighs
- skin tags, or tiny excess flaps of skin in the armpits or neck area
- pelvic pain
- anxiety or depression due to appearance and/or infertility
- sleep apnea—excessive snoring and times when breathing stops while asleep
Why do women with polycystic ovary syndrome (PCOS) have trouble with their menstrual cycle?
The ovaries are two small organs, one on each side of a woman's uterus. A woman's ovaries have follicles, which are tiny sacs filled with liquid that hold the eggs. These sacs also are called cysts. Each month about 20 eggs start to mature, but usually only one matures fully. As this one egg grows, the follicle accumulates fluid in it. When that egg matures, the follicle breaks open to release it. The egg then travels through the fallopian tube for fertilization. When the single egg leaves the follicle, ovulation takes place.
In women with PCOS, the ovary doesn't make all of the hormones it needs for any of the eggs to fully mature. Follicles may start to grow and build up fluid. But no one follicle becomes large enough. Instead, some follicles may remain as cysts. Since no follicle becomes large enough and no egg matures or is released, ovulation does not occur and the hormone progesterone is not made. Without progesterone, a woman's menstrual cycle is irregular or absent. Plus, the cysts make male hormones, which also prevent ovulation.
Does polycystic ovary syndrome (PCOS) change at menopause?
Yes and no. Because PCOS affects many systems in the body, many symptoms persist even though ovarian function and hormone levels change as a woman nears menopause. For instance, excessive hair growth continues, and male pattern baldness or thinning hair gets worse after menopause. Also, the risks of complications from PCOS, such as heart attack, stroke and diabetes, increase as a woman gets older.
What tests are used to diagnose polycystic ovary syndrome (PCOS)?
There is no single test to diagnose PCOS. Your doctor will take a medical history, perform a physical exam, and possibly take some tests to rule out other causes of your symptoms. During the physical exam the doctor will want to measure your blood pressure, body mass index (BMI), and waist size. He or she also will check out the areas of increased hair growth, so try to allow the natural hair growth for a few days before the visit. Your doctor might want to do a pelvic exam to see if your ovaries are enlarged or swollen by the increased number of small cysts. A vaginal ultrasound also might be used to examine the ovaries for cysts and check out the endometrium, the lining of the uterus. The uterine lining may become thicker if your periods are not regular. You also might have blood taken to check your hormone levels and to measure glucose (sugar) levels.
How is polycystic ovary syndrome (PCOS) treated?
Because there is no cure for PCOS, it needs to be managed to prevent problems. Treatment goals are based on your symptoms, whether or not you want to become pregnant, and lowering your chances of getting heart disease and diabetes. Many women will need a combination of treatments to meet these goals.
Some treatments for PCOS include:
- Birth control pills. For women who don't want to become pregnant, birth control pills can control menstrual cycles, reduce male hormone levels, and help to clear acne. However, the menstrual cycle will become abnormal again if the pill is stopped. Women may also think about taking a pill that only has progesterone, like Provera®, to control the menstrual cycle and reduce the risk of endometrial cancer. (See Does polycystic ovary syndrome (PCOS) put women at risk for other health problems?) But progesterone alone does not help reduce acne and hair growth.
- Diabetes medications. The medicine metformin (Glucophage®) is used to treat type 2 diabetes. It also has been found to help with PCOS symptoms, although it is not FDA-approved for this use. Metformin affects the way insulin controls blood glucose (sugar) and lowers testosterone production. Abnormal hair growth will slow down, and ovulation may return after a few months of use. Recent research has shown metformin to have other positive effects, such as decreased body mass and improved cholesterol levels. Metformin will not cause a person to become diabetic.
- Fertility medications. Lack of ovulation is usually the reason for fertility problems in women with PCOS. Several medications that stimulate ovulation can help women with PCOS become pregnant. Even so, other reasons for infertility in both the woman and man should be ruled out before fertility medications are used. Also, there is an increased risk for multiple births (twins, triplets) with fertility medications. For most patients, clomiphene citrate (Clomid®, Serophene®) is the first choice therapy to stimulate ovulation. If this fails, metformin taken with clomiphene is usually tried. When metformin is taken along with fertility medications, it may help women with PCOS ovulate on lower doses of medication. Gonadotropins (goe-NAD-oh-troe-pins) also can be used to stimulate ovulation. These are given as shots. But gonadotropins are more expensive and there are greater chances of multiple births compared to clomiphene. Another option is in vitro fertilization (IVF). IVF offers the best chance of becoming pregnant in any one cycle and gives doctors better control over the chance of multiple births. But, IVF is very costly.
- Medicine for increased hair growth or extra male hormones. Medicines called anti-androgens may reduce hair growth and clear acne. Spironolactone (speer-on-oh-lak-tone) (Aldactone®), first used to treat high blood pressure, has been shown to reduce the impact of male hormones on hair growth in women. Finasteride (Propecia®), a medicine taken by men for hair loss, has the same effect. Anti-androgens often are combined with oral contraceptives.
- Before taking Aldactone®, tell your doctor if you are pregnant or plan to become pregnant. Do not breastfeed while taking this medicine. Women who may become pregnant should not handle Propecia®.
- Vaniqa® cream also reduces facial hair in some women. Other treatments such as laser hair removal or electrolysis work well at getting rid of hair in some women. A woman with PCOS can also take hormonal treatment to keep new hair from growing.
- Surgery. "Ovarian drilling" is a surgery that brings on ovulation. It is sometimes used when a woman does not respond to fertility medicines. The doctor makes a very small cut above or below the navel and inserts a small tool that acts like a telescope into the abdomen. This is called laparoscopy. The doctor then punctures the ovary with a small needle carrying an electric current to destroy a small portion of the ovary. This procedure carries a risk of developing scar tissue on the ovary. This surgery can lower male hormone levels and help with ovulation. But these effects may only last a few months. This treatment doesn't help with loss of scalp hair and increased hair growth on other parts of the body.
- Lifestyle modification. Keeping a healthy weight by eating healthy foods and exercising is another way women can help manage PCOS. Many women with PCOS are overweight or obese. Eat fewer processed foods and foods with added sugars and more whole-grain products, fruits, vegetables, and lean meats to help lower blood sugar (glucose) levels, improve the body's use of insulin, and normalize hormone levels in your body. Even a 10 percent loss in body weight can restore a normal period and make a woman's cycle more regular.
How does polycystic ovary syndrome (PCOS) affect a woman while pregnant?
There appears to be higher rates of miscarriage, gestational diabetes, pregnancy-induced high blood pressure (pre-eclampsia), and premature delivery in women with PCOS. Researchers are studying how the diabetes medicine metformin can prevent or reduce the chances of having these problems while pregnant. Metformin also lowers male hormone levels and limits weight gain in women who are obese when they get pregnant.
Metformin is a FDA pregnancy category B drug. It does not appear to cause major birth defects or other problems in pregnant women. But, there have been no studies of metformin on pregnant women to confirm its safety. Talk to your doctor about taking metformin during pregnancy or if you are trying to become pregnant. Also, metformin is passed through milk in breastfeeding mothers. Talk with your doctor about metformin use if you are a nursing mother.
Does polycystic ovary syndrome (PCOS) put women at risk for other health problems?
Women with PCOS have greater chances of developing several serious, life-threatening diseases, including type 2 diabetes, cardiovascular disease (CVD), and cancer. Recent studies found that:
- More than 50 percent of women with PCOS will have diabetes or pre-diabetes (impaired glucose tolerance) before the age of 40.
- Women with PCOS have a four to seven times higher risk of heart attack than women of the same age without PCOS.
- Women with PCOS are at greater risk of having high blood pressure.
- Women with PCOS have high levels of LDL (bad) cholesterol and low levels of HDL (good) cholesterol.
The chance of getting endometrial cancer is another concern for women with PCOS. Irregular menstrual periods and the absence of ovulation cause women to produce the hormone estrogen, but not the hormone progesterone. Progesterone causes the endometrium to shed its lining each month as a menstrual period. Without progesterone, the endometrium becomes thick, which can cause heavy bleeding or irregular bleeding. Over time, this can lead to endometrial hyperplasia, when the lining grows too much, and cancer.
I have PCOS. What can I do to prevent complications?
Getting your symptoms under control at an earlier age can help to reduce your chances of having complications like diabetes and heart disease. Talk to your doctor about treating all your symptoms, rather than focusing on just one aspect of your PCOS, such as problems getting pregnant. Also, talk to our doctor about getting tested for diabetes regularly. Eating right, exercising, and not smoking also will help to reduce your chances of having other health problems.
How can I cope with the emotional effects of PCOS?
Having PCOS can be difficult. Many women are embarrassed by their appearance. Others may worry about being able to get pregnant. Some women with PCOS might get depressed. Getting treatment for PCOS can help with these concerns and help boost a woman's self-esteem. Support groups located across the United States and on-line also can help women with PCOS deal with the emotional affects.
Labels: Menstrual Disorder
 New life begins when an egg from a woman is fertilised by sperm from a man. Ovulation occurs around 14 days before the start of the menstrual period, when an egg (ovum) is released from one of the ovaries. The egg is swept into the nearby fallopian tube and ushered towards the uterus (womb). If the egg is fertilised on its journey, it lodges in the womb lining (endometrium). Pregnancy then begins. The odds of a young fertile couple conceiving by having sexual intercourse around the time of ovulation are approximately one in five every month. A couple isn’t thought to have fertility problems until they have tried, and failed, to conceive for one year. Approximately 20 per cent of couples experience difficulties. In most cases, the couple can be helped with assisted reproductive technologies. Around 40 per cent of fertility problems originate in the woman. Female fertility problems include failure to ovulate, and abnormalities of the fallopian tubes or uterus.
New life begins when an egg from a woman is fertilised by sperm from a man. Ovulation occurs around 14 days before the start of the menstrual period, when an egg (ovum) is released from one of the ovaries. The egg is swept into the nearby fallopian tube and ushered towards the uterus (womb). If the egg is fertilised on its journey, it lodges in the womb lining (endometrium). Pregnancy then begins. The odds of a young fertile couple conceiving by having sexual intercourse around the time of ovulation are approximately one in five every month. A couple isn’t thought to have fertility problems until they have tried, and failed, to conceive for one year. Approximately 20 per cent of couples experience difficulties. In most cases, the couple can be helped with assisted reproductive technologies. Around 40 per cent of fertility problems originate in the woman. Female fertility problems include failure to ovulate, and abnormalities of the fallopian tubes or uterus.
Ovulation problems
 The menstrual cycle is orchestrated by a number of glands and their hormones working in harmony. For ovulation to occur, a part of the brain called the hypothalamus prompts the nearby pituitary gland to secrete hormones that trigger the ovaries to ripen eggs. Irregular or absent periods indicate that ovulation may be irregular or absent too. The age of the woman is a significant fertility factor. The chance of pregnancy for a woman aged 40 years and over is only five per cent per menstrual cycle. It is thought that ageing eggs may be the cause. A woman is born with her entire egg supply and, as time passes, these eggs become less viable. Other difficulties for the older woman include increased risk of miscarriage and genetic abnormalities in the unborn baby.
The menstrual cycle is orchestrated by a number of glands and their hormones working in harmony. For ovulation to occur, a part of the brain called the hypothalamus prompts the nearby pituitary gland to secrete hormones that trigger the ovaries to ripen eggs. Irregular or absent periods indicate that ovulation may be irregular or absent too. The age of the woman is a significant fertility factor. The chance of pregnancy for a woman aged 40 years and over is only five per cent per menstrual cycle. It is thought that ageing eggs may be the cause. A woman is born with her entire egg supply and, as time passes, these eggs become less viable. Other difficulties for the older woman include increased risk of miscarriage and genetic abnormalities in the unborn baby.
Polycystic ovary syndrome
At the time of ovulation, the ovaries produce small cysts or blisters called follicles. Typically, one follicle ripens to release an egg. In polycystic ovary syndrome, the follicles fail to ripen, forming little cysts at the periphery of the ovary and often releasing male sex hormones.
Problems with the fallopian tubes
The sperm fertilises the egg on its journey down the fallopian tube. A blocked or scarred fallopian tube may impede the egg’s progress, preventing it from meeting up with sperm. A surgical procedure called laparoscopy can be used to check for obstructions.
Problems with the uterus
The fertilised egg lodges in the lining of the uterus. Some uterine problems that can hamper implantation include:
- Fibroids - non-malignant tumours inside the womb.
- Polyps - overgrowths of the endometrium, which can be prompted by the presence of fibroids.
Problems with the cervix
At the top of the vagina is the neck or entrance to the uterus, called the cervix. The cervix has a small central hole (the os) that allows passage of menstrual fluid and other secretions out of the uterus. Ejaculated sperm must travel through the cervix to access the uterus and fallopian tubes. Cervical mucus around the time of ovulation is normally thin and watery so that sperm can swim through it. However, thick or poor quality cervical mucus can hinder the sperm.
Endometriosis
Endometriosis is a condition in which cells from the lining of the uterus (the endometrium) migrate to other parts of the pelvis. This can also lead to fertility problems.
Idiopathic infertility
For around one in 10 couples investigated for infertility, no cause is found. This is called ‘unexplained’ or ‘idiopathic’ infertility.
Diagnosis methods
Investigating suspected infertility requires a number of tests for both the woman and her partner. Tests for the woman may include:
- Blood tests - to check for the presence of ovulation hormones.
- Laparoscopy - a ‘keyhole’ surgical procedure in which an instrument is inserted though a small incision in the abdomen so that the reproductive organs can be examined.
- Ultrasound tests - to check for the presence of fibroids.
A semen analysis may also be done to make sure that the male partner is fertile.
Treatment options
Treatment options for female infertility depend on the cause, but may include:
- Hormone therapy - to prompt ovulation.
- Surgery - to unblock fallopian tubes, treat endometriosis or remove fibroids.
- Assisted reproductive technologies - including in vitro fertilisation (IVF), where conception occurs in the laboratory and the fertilised egg is later implanted in the prepared uterus.
Treatment for female infertility does not bring about conception in all cases.
Things to remember
- Around 40 per cent of fertility problems originate in the woman.
- Female fertility problems include failure to ovulate, blockages in the fallopian tubes, and abnormalities of the uterus, such as fibroids or endometriosis.
Labels: Infertility
Visitor
Labels
- Carcinoma (2)
- Dysmenorrhoea (4)
- Endometriosis (4)
- Female Genital Infection (3)
- Fluor Albus (4)
- General (3)
- Genital Prolapse (4)
- Gynecology (8)
- Infectious Disease in Pregnancy (13)
- Infertility (10)
- Menopause (3)
- Menstrual Disorder (10)
- Myoma Uteri (3)
- Obstetrics (13)
- Pelvic Floor (4)
- Pelvic Inflamatory Disease (3)
- Physiology of Human Reproductive System (4)
- Pregnancy (2)
- Sexually Transmitted Disease (6)
- Uterine Bleeding (4)
Followers
Facebook Badge
Copyright © 2009 Complicated Girl. All Rights Reserved.