Information Site About Reproductive System
About Me
Blog Archive
-
▼
2009
(58)
-
▼
December
(17)
- Syphilis During Pregnancy
- STDs and Pregnancy - Fact Sheet
- URINARY TRACT INFECTIONS in PREGNANCY
- GROUP B STREPTOCOCCUS INFECTION and PREGNANCY
- SWINE FLU and PREGNANCY
- GENITAL HERPES IN PREGNANCY
- LISTERIA and PREGNANCY
- REPIRATORY INFECTIONS DURING PREGNANCY
- HEPATITIS IN PREGNANCY
- CYTOMEGALOVIRUS
- CHLAMYDIA
- RUBELLA
- TOXOPLASMOSIS
- RECTOCELE
- CYSTOCELE
- PROLAPSE OF THE UTERUS
- PELVIC FLOOR
-
▼
December
(17)
Tuesday, December 1, 2009
The rectum is the temporary storage area for bowel motions, and makes up the last 20cm or so of the large bowel.
A rectocele occurs when the rectum pushes the back wall of the vagina forward, causing a prominent bulge into the vagina.
Risk factors include difficult childbirth and the use of forceps during delivery, but women who have never had children can also develop rectocele.
The degree of severity varies; for example, in mild cases the rectocele may be felt as a small bulge high inside the vagina while, in severe cases, the bulge may be hanging outside of the vagina. Milder cases can be treated by measures such as management of constipation, Kegel exercises to strengthen the pelvic floor and the insertion of a vaginal pessary to prop up the pelvic organs. Surgery may be needed in severe cases.
Symptoms
The symptoms of rectocele may be vaginal, rectal or both, and can include:
- A sensation of pressure within the pelvis
- The feeling that something is falling down or falling out within the pelvis
- Symptoms are worsened by standing up and eased by lying down
- Lower abdominal pain
- Lower back pain
- A bulging mass felt inside the vagina
- Vaginal bleeding that’s not related to the menstrual cycle
- Painful or impossible vaginal intercourse
- Constipation
- Problems with passing a bowel motion, since the stool becomes caught in the rectocele
- The feeling that the bowel isn’t completely emptied after passing a motion
- Faecal incontinence (sometimes).
Rectovaginal septum explained
The pelvic organs are supported by the pelvic floor muscles. Structures including ligaments and connective tissue help to keep the pelvic organs tethered in place. In women, the front wall of the rectum is situated behind the rear wall of the vagina.
The front wall of the rectum and rear wall of the vagina, and the thin layer of tissue between them, are together called the rectovaginal septum (or wall). This wall can become weak or stretched by pressure such as childbirth or straining while going to the toilet and by ageing. A weak or thinned rectovaginal septum allows the front wall of the rectum to bulge into the vagina.
A range of causes
Some of the events that may weaken or thin the rectovaginal septum and cause a rectocele include:
- Vaginal (normal) childbirth
- Giving birth to multiple babies
- A long and difficult labour
- Assisted delivery during childbirth, including the use of forceps
- Tearing during childbirth, particularly if the tear extended from the vagina to the anus
- Episiotomy (a surgical cut made to enlarge the vaginal opening during childbirth to avoid injury to mother and baby), particularly if the cut extends to the anus
- Hysterectomy
- Pelvic surgery
- Chronic constipation
- Straining to pass bowel motions
- Advancing age, as older women are more prone to rectocele.
Related problems
A rectocele sometimes occurs by itself. In other cases, it may present alongside other abnormalities including:
- CYSTOCELE - the bladder protrudes into the vagina.
- ENTEROCELE- the small intestines push down into the vagina.
- UTERINE PROLAPSE - the cervix and uterus drop down into the vagina and may protrude out of the vaginal opening.
- VAGINAL PROLAPSE - in cases of severe uterine prolapse, the vagina may slide out of the body too.
- RECTAL PROLAPSE - the rectum protrudes through the anus.
Diagnosis methods
Rectocele is diagnosed using a number of tests including:
- Pelvic examination
- Special x-ray (proctogram or defaecagram).
Treatment options
Generally speaking, a rectocele with no obvious symptoms doesn’t need medical treatment, but it is wise to pay attention to diet and other lifestyle factors that contribute to constipation. Treatment options may include:
- High fibre diet
- Fibre supplements
- At least six to eight glasses of water per day
- Stool softeners (don’t use laxatives)
- Instruction on how to help yourself to pass a bowel motion; for example, you may be advised to gently press a finger against the rear wall of the vagina while toileting
- Don’t strain on the toilet
- Hormone replacement therapy for postmenopausal women
- Pelvic floor (‘Kegel’) exercises
- The insertion of a pessary, which is a ring-like device worn high in the vagina that helps to support the pelvic organs.
Surgery
Surgery may be needed if the rectocele doesn’t respond to other treatments and is causing symptoms. Unfortunately, the rectocele will recur after operation in about 10 per cent of cases. Depending on individual factors, such as the severity of the rectocele and the presence of other prolapsed structures, the operation can be performed in a number of ways, including:
- Through the vagina
- Through the anus
- Through the area between the vagina and anus (perineum)
- Through the abdomen
- In some cases, a combination of surgical techniques may be necessary.
Things to remember
- Some of the causes of a rectocele include vaginal childbirth, hysterectomy, pelvic surgery and chronic constipation.
- A rectocele may occur by itself or present alongside other pelvic abnormalities, such as a prolapsed bladder (cystocele).
- Surgery may be needed if the rectocele doesn’t respond to simpler treatments.
Labels: Genital Prolapse, Gynecology, Pelvic Floor
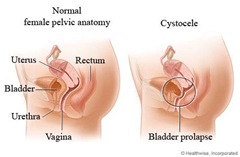
A cystocele is when the bladder bulges into the vagina.
Risk factors include vaginal childbirth, regularly straining on the toilet to pass bowel motions, obesity, smoking and chronic lung diseases with coughing.
Postmenopausal women are more susceptible to cystocele. This is because the sex hormone, oestrogen, helps to keep the muscles of the vagina and bladder – the pelvic floor muscles – in good tone. Once oestrogen levels drop, these muscles become thinner, weaker and less elastic. The vaginal skin stretches, which may allow the bladder to bulge into the vagina.
A cystocele can occur by itself or it may happen along with other abnormalities such as a rectocele (when the rectum protrudes into the vagina) or a uterine prolapse (when the uterus and cervix drop down to the vaginal entrance).
Treatment options include pelvic floor exercises, oestrogen therapy, inserting a pessary into the vagina to hold up the pelvic organs, and surgery. Other names for cystocele include prolapse of the bladder and ‘fallen’ bladder.
Symptoms
The symptoms of cystocele depend on individual factors, such as the severity of the condition, but can include:
- Stress incontinence – urine leaks when coughing, sneezing, laughing, standing up, running or walking
- Inability to completely empty the bladder after going to the toilet
- Recurring urinary tract infections (UTIs)
- Urination problems, such as straining to get urine flow started or an unusually slow flow of urine that tends to stop and start
- A sensation of fullness or pressure inside the vagina
- A bulging mass felt on the front wall of the vagina
- In severe cases, the vagina and the bladder protrude out of the vaginal entrance.
Grades of severity
A cystocele is graded on its degree of severity:
- GRADE 1 – the bladder protrudes a little way into the vagina.
- GRADE 2 – the bladder protrudes so far into the vagina that it is close to the vaginal opening.
- GRADE 3 – the bladder protrudes out of the vagina.
A range of causes
The vagina and bladder are held apart by tissue known as the pubocervical fascia. Thinning, weakening or tearing of the pubocervical fascia, and poor tone of the supporting muscles and ligaments, allow the bladder to drop against the vaginal wall. Some of the events that may cause or contribute to the development of a cystocele include:
- Vaginal childbirth
- Repeated heavy lifting
- Habitually straining to pass bowel motions
- The drop in oestrogen levels that occurs at menopause.
Diagnosis
Cystocele is diagnosed using a number of tests including:
- MEDICAL HISTORY – to check for possible risk factors.
- PHYSICAL EXAMINATION– cases of grade 2 or 3 cystocele can be easily diagnosed by vaginal examination.
- VOIDING CYSTOURETHROGRAM – a rarely used special x-ray that is taken while the patient is urinating. This test reveals whether the flow of urine is affected by the cystocele and if there is significant urine left in the bladder after passing urine (residual urine).
- OTHER TESTS– such as a bladder or pelvic ultrasound, a urodynamics investigation or x-rays to exclude other possible causes of urinary problems.
Treatment
Treatment for cystocele depends on the severity of the condition, but can include:
- MILD CASES – when there are no symptoms, treatment may be unnecessary. Regular monitoring is needed to make sure the cystocele doesn’t worsen. The doctor may advise a few lifestyle changes to prevent the condition getting worse, including doing pelvic floor exercises to strengthen the pelvic floor muscles.
- MODERATE CASES – a pessary is a small ring-like device that’s inserted high in the vagina. This is used temporarily in younger women and helps to keep the bladder in place. Health risks of long-term pessary use include infection and ulceration. This is more likely to be used in elderly women who are considered unfit for surgery due to chronic medical conditions.
- SEVERE CASES where symptoms impair quality of life. There are many different surgical techniques now available.
Pelvic floor physiotherapy
Pelvic floor exercises help to increase the strength of the pelvic floor muscles. They may reduce the symptoms felt as the result of a moderate to large cystocele. These exercises may also reduce symptoms of stress incontinence, which is often associated with a cystocele. It is important to learn to do the exercises correctly to gain the most benefit. There are specially trained physiotherapists or other health professionals available to help teach the correct techniques.
Surgery
Surgery for cystocele repair is usually done under general anaesthesia but also may be done under spinal or epidural anaesthesia. There are now many different types of surgery available depending on the symptoms a woman has. Traditionally, the vaginal wall is cut, the bladder is pushed away from the vagina and the excess vaginal tissue is removed. The bladder is supported by sutures into the pubocervical fascia and then the vagina is closed.
Mesh, graft or tape may be used to hold the bladder and urethra in place. Some procedures may be performed laparoscopically. Other procedures performed during the operation depend on individual factors: for example, a vagina overstretched by childbirth may be tightened.
A urinary catheter may be worn for between one and six days following surgery depending on the type of operation performed. Full recovery takes around four to six weeks.
Self-care suggestions
Your doctor may advise that you make a few lifestyle changes to prevent the cystocele from worsening or recurring after surgery. These suggestions may include:
- Don’t lift heavy objects.
- Increase the amount of fibre in your diet to prevent constipation and straining.
- Drink between six and eight glasses of water each day. Not drinking enough water makes stools hard, dry and difficult to pass.
- Exercise daily to help keep you regular.
- Use stool softeners, which may help in the short term.
- Avoid straining on the toilet for either bowels or bladder; use the hissing or sighing technique.
- Perform pelvic floor exercises daily to strengthen the muscles supporting the pelvic organs. You may need instruction from your doctor or other health care professional, such as a pelvic floor rehabilitation physiotherapist.
- Always squeeze up your pelvic floor muscles before you lift, cough, laugh or sneeze.
- If you are postmenopausal, your doctor may recommend hormone therapy, usually in the form of local oestrogen preparations such as a cream or a vaginal tablet, to help tone the muscles supporting the vagina and bladder.
- Seek medical advice for any condition that causes coughing and sneezing such as asthma, chest infections and hay fever.
- Keep yourself within a healthy weight range.
- Avoid sit-ups. Learn how to strengthen your deep abdominal muscles, but avoid straining.
Point to remember
- A cystocele is when the bladder bulges out into an overstretched vagina.
- Risk factors include vaginal childbirth and regularly straining on the toilet to pass bowel motions.
- Severe cases of cystocele need surgical repair.
Labels: Genital Prolapse, Gynecology, Pelvic Floor
Prolapse of the uterus
The uterus (womb) is an organ of the female reproductive system.
It is shaped like an upside down pear and is located inside the pelvis.
The uterus, bladder and bowel are supported by a tight hammock of muscles slung between the tailbone (coccyx) and the pubic bone. These muscles are known as the PELVIC FLOOR, or the LEVATOR ANI MUSCLES.
Ligaments and connective tissue also anchor the uterus in place. If these tissues are weakened or damaged, the uterus can slip down into the vagina.
Common causes of uterine prolapse include CHILDBIRTH – OBESITY – CHRONIC CONSTIPATION and POSTMENOPAUSE .
Other names for uterine prolapse include PUDENDAL HERNIA and PELVIC FLOOR HERNIA
Treatment options include special muscle strengthening exercises. Surgery may be needed in severe cases.
Symptoms
The symptoms of uterine prolapse include:
- A sensation of heaviness in the vagina
- A distinct lump or bulge in the vagina
- Tissue protruding out of the vagina
- Persistent aching in the lower back
- Trouble passing urine
- Frequent urinary tract infections
- Greater than normal amounts of vaginal discharge
- Painful sexual intercourse.
Degrees of prolapse
Uterine prolapse is categorised by the degree of tissue protruding into the vagina. In most cases, other pelvic organs (such as the bladder or bowel) are also prolapsed into the vagina, and the ovaries sit lower than normal inside the pelvis. The three categories of uterine prolapse are:
- FIRST DEGREE (mild) - the neck of the uterus (cervix) protrudes into the lowest third of the vagina.
- SECOND DEGREE (moderate) - the cervix protrudes to the opening of the vagina.
- THIRD DEGREE (severe) - the whole uterus protrudes out of the vagina.
A range of causes
The pelvic floor and associated supporting ligaments can be weakened or damaged in many ways including:
- Pregnancy, especially in the case of multiple babies such as twins or triplets.
- Vaginal childbirth, especially if the baby was large or delivered quickly, or if there was a prolonged pushing phase.
- Obesity.
- Chronic constipation and associated straining to pass motions.
- Low levels of the sex hormone oestrogen after menopause.
- Constant coughing associated with conditions such as chronic bronchitis or asthma.
- Fibroids.
- In rare cases, pelvic tumour.
Pelvic floor exercises
In mild to moderate cases, special exercises of the pelvic floor can correct uterine prolapse. Familiarising yourself with the muscles of each orifice gives you a better chance of performing the exercises correctly. To identify the muscles of your vagina, insert one or two fingers and squeeze them. For your urethra, halt the flow of urine in midstream, but do not do this on a regular basis. Finally, familiarise yourself with the muscles of your anus by pretending to stop yourself from breaking wind. Consult with your doctor, physiotherapist or health care professional to ensure correct performance. Basically, the pelvic floor exercises include:
- As a warm-up, direct your attention to your pelvic floor. Gradually squeeze all three sphincters and increase the tension until you have contracted the muscles as hard as you can. Release slowly and gently.
- Squeeze slowly and hold for five to 10 seconds. Release slowly. Repeat 10 times. Relax for 10 seconds in between each one.
- Perform quick, short strong squeezes. Repeat 10 times.
- Remember to squeeze your muscles whenever you sneeze or cough.
VAGINAL PESSARY
A device shaped like a doughnut may be inserted into the vagina and positioned to prop the cervix and uterus. Side effects include irritating discharge and an increased risk of ulceration. Vaginal pessaries are considered a short term solution, and pelvic floor exercises and perhaps surgery will still be needed in the longer term.
VAGINAL SURGERY
In moderate to severe cases, the prolapse may have to be surgically repaired. In laparoscopic surgery, slender instruments are inserted through the navel. The uterus is pulled back into its proper place and reattached to supporting ligaments using permanent stitches. Over time, scar tissue grows over these stitches and further strengthens the repair. The operation may be performed abdominally in some circumstances. In around nine out of 10 cases, corrective surgery is successful.
Prevention techniques
Some women are at increased risk of uterine prolapse. Simple preventive measures include:
- PREGNANCY - pelvic floor exercises throughout the duration of pregnancy.
- VAGINALCHILDBIRTH - a well-timed episiotomy (an intentional and controlled cut of the skin between the vagina and anus) to prevent tearing and trauma to the pelvic floor muscles caused by the baby’s emerging head, and post-partum pelvic floor exercises.
- POSTMENOPAUSE - oestrogen creams to boost flagging hormone levels, and pelvic floor exercises.
- OBESITY - loss of excess body fat with dietary modifications and regular exercise, and pelvic floor exercises.
- OTHER CONDITION - treat underlying disorders (such as asthma, chronic bronchitis or chronic constipation) in consultation with your doctor.
- CHRONIC CONSTIPATION - drink plenty of fluid, eat lots of fruit, vegetables and fibre, and relax your tummy muscles to avoid straining when using your bowels.
Point to remember
- Uterine prolapse occurs when weakened or damaged muscles and ligaments allow the uterus to slip into the vagina.
- Common causes include pregnancy, childbirth, hormonal changes after menopause, obesity and chronic constipation.
- Treatment options include pelvic floor exercises and vaginal surgery.
Labels: Genital Prolapse, Gynecology, Pelvic Floor
PELVIC FLOOR ~ pelvic diaphragm
The pelvic floor muscles are tightly slung between the tailbone (coccyx) and the pubic bone, and support the bowel, bladder, uterus and vagina.
Muscular bands (sphincters) encircle the urethra, vagina and anus as they pass through the pelvic floor.
When the pelvic floor muscles are contracted, the internal organs are lifted and the sphincters tighten the openings of the vagina, anus and urethra. Relaxing the pelvic floor allows passage of urine and faeces.
If the muscles are weakened, the internal organs are no longer fully supported and you may not be able to control your urine. Common causes of a weakened pelvic floor include childbirth, obesity and the associated straining of chronic constipation. Pelvic floor exercises are designed to improve muscle tone and prevent the need for corrective surgery.
Symptoms
The symptoms of a weakened pelvic floor include:
- Leaking small amounts of urine when coughing, sneezing, laughing or running
- Failing to reach the toilet in time
- Uncontrollably breaking wind from either the anus or vagina when bending over or lifting
- Reduced sensation in the vagina
- Backache
- Tampons that dislodge or fall out
- A distinct swelling at the vaginal opening
- A sensation of heaviness in the vagina.
Common causes
The pelvic floor can be weakened in many ways, including:
- The weight of the uterus during pregnancy
- Vaginal childbirth, which overstretches the muscles
- The pressure of obesity
- Chronic constipation and associated straining to pass motions
- Constant coughing
- Some forms of surgery that require cutting the muscles
- Lower levels of oestrogen after menopause.
Complications of a weakened pelvic floor
LOSS OF BLADDER CONTROL a common symptom of a weakened pelvic floor ( URINE INCONTINENCE ) . Some people experience BOWEL INCONTINENCE , which means they can’t always control the passage of wind or faeces ( INCONTINECE ALVI ).
Weak pelvic floor muscles can also cause SEXUAL DIFFICULTIES such as reduced vaginal sensation.
In severe cases, the internal organs supported by the pelvic floor, including the bladder and uterus, can slide down into the vagina. This is called a PROLAPSE. A distinct bulge in the vagina and deep, persistent vaginal aching are common symptoms.
Familiarising yourself with the pelvic floor
Pelvic floor exercises are designed to strengthen the muscles. Each sphincter (vaginal, urethral, anal) should be exercised, so you need to familiarise yourself with these muscles in order to contract them at will. If the pelvic floor is especially weak, it may be difficult to detect any muscular contractions at first.
Suggestions on identifying your sphincters include:
- VAGINAL - one or two fingers into your vagina and try to squeeze them.
- URETHRAL - you urinating, try stopping the flow in midstream. This should only be done to identify the sphincters. Do not do it on a regular basis.
- ANAL – pretend you are trying to stop yourself from breaking wind and squeeze tightly.
The exercises
You can perform these exercises lying down, sitting or standing. Ideally, aim for five or six sessions every day while you are learning the exercises. After you have a good understanding of how to do the exercises, three sessions each day is enough.
Before you start, direct your attention to your pelvic floor muscles. Try to relax your abdominal muscles. Don’t bear down or hold your breath. Gradually squeeze all three sphincters and increase the tension until you have contracted the muscles as hard as you can. Release gently and slowly. Then perform the exercises, which include:
- Squeeze slowly and hold as strongly as you can for 5 to 10 seconds while breathing normally. Release slowly. Repeat 10 times. Relax for 5 to 10 seconds between each one.
- Perform quick, short, strong squeezes. Repeat 10 times.
- Remember to squeeze the muscles whenever you clear your throat or cough.
Professional help
It is important to perform these exercises correctly. You can consult with your doctor, physiotherapist or continence advisor to ensure proper performance. It may take weeks or months before you notice a substantial improvement. In severe cases, pelvic floor exercises aren’t enough to solve the problem and surgery may be needed. Be guided by your health care professional.
Other considerations
You can further improve the strength of your pelvic floor in many ways, including:
- Lose excess body fat
- Cure constipation by including more fruit, vegetables, fibre and water in your daily diet
- Seek medical attention for a chronic cough.
Key To Remember
- The pelvic floor muscles support the bladder, uterus and bowel.
- The pelvic floor can be weakened by pregnancy, childbirth, obesity and the straining of chronic constipation.
- Pelvic floor exercises are designed to improve muscle strength.
Labels: Genital Prolapse, Gynecology, Pelvic Floor
Monday, November 30, 2009
| |
Hysterectomy is the surgical removal of a woman's uterus. It may also involve the removal of the fallopian tubes and ovaries. Once a hysterectomy is performed, a woman can no longer have children or menstrual periods.
Hysterectomy is used to treat a number of conditions, such as excessive menstrual bleeding and cancer. In Australia, around 30,000 women undergo this operation every year.
Conditions that may require hysterectomy
A hysterectomy may be performed to correct various gynaecological problems including:
- Heavy, irregular or abnormal menstrual bleeding
- Fibroids
- Endometriosis
- Uterine prolapse
- Cancer of the uterus, ovary or cervix
- Pelvic inflammatory disease.
Medical issues to consider
Apart from cancer, many of the gynaecological conditions assisted by hysterectomy may also be successfully treated using other methods. If, after discussion of all options with your doctor, you choose to have a hysterectomy, there are several things that your doctor should discuss with you before the operation. These include:
- Your medical history (as some pre-existing conditions may influence decisions on surgery and anaesthetics).
- The pros and cons of abdominal surgery versus vaginal surgery.
- Your support options after surgery.
- Your feelings about the surgery.
You will have a range of tests, including a complete blood count test to check for problems such as anaemia.
Operation procedure
You will have an intravenous drip inserted into a vein in your hand or arm, and will be given a general anaesthetic. The operation may be performed via a lower abdominal incision (cut) or through the vagina.
Abdominal hysterectomy
For an abdominal hysterectomy, a cut is usually made horizontally along your pubic hairline (and your pubic hair will be shaved around the incision). For most women, this results in a small scar. Some patients may need a vertical incision in the lower abdomen.
Vaginal hysterectomy
A vaginal hysterectomy is performed through an incision (cut) at the top of the vagina. This may or may not involve the use of a laparoscope. A laparoscope is a slender instrument used in 'keyhole' surgery. During a laparoscopic assisted vaginal hysterectomy, surgery is performed via three or four small incisions in the abdomen. It is completed through the vagina.
Vaginal hysterectomy is a preferred option for many women as it avoids the need for a long abdominal cut. An abdominal procedure is generally recommended when large fibroids or cancer is present.
Types of hysterectomy
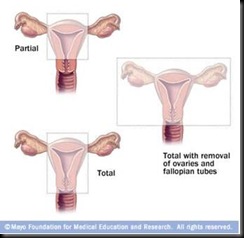
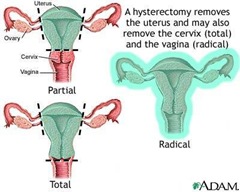
There are four variations of hysterectomy, including:
| |
- TOTAL HYSTERECTOMY - the entire uterus and cervix is removed, but the ovaries are retained.
- SUBTOTAL (partial)HYSTERECTOMY- the uterus is removed, but the cervix may be retained. While removal of the cervix is generally advised because it is a potential cancer site in the body, some women consider that it serves a purpose during penetrative sex. If the cervix is kept, regular Pap smears are necessary.
- HYSTERECTOMY and BILATERAL SALPHYNGOOPHARECTOMY - the uterus, fallopian tubes and ovaries are removed. This operation is performed if cancer of the ovaries or the uterus has been diagnosed. It may also be performed for severe infection or endometriosis.
- RADICAL HYSTERECTOMY - the most extensive version of the operation. It involves the removal of the uterus, fallopian tubes, ovaries, upper part of the vagina, and associated pelvic ligaments and lymph nodes. This may be performed if cancer of the cervix, ovaries or uterus is present.
Immediately after the operation
After the operation, you can expect:
- There will be some soreness around the operation site - your doctor will prescribe pain-killing medication for you.
- You may experience 'wind' pain for a few days.
- Depending on the procedure and your condition, the intravenous tube in your arm will be removed sometime during the first few days.
- The catheter (drainage tube) in your bladder is usually removed within 24 hours of surgery, unless the bladder was traumatised during the procedure.
- As soon as possible, you will be encouraged to get out of bed and go for short walks around the ward.
- Depending on the type of surgery, you can expect a hospital stay of between two and seven days.
- Recovery is generally faster after vaginal surgery than abdominal surgery.
Following surgery, it is important to start pelvic floor and abdominal exercises as soon as possible. These exercises strengthen the muscles in the pelvis and help maintain normal bladder function and vaginal muscle tone. Your doctor or physiotherapist will let you know how soon you can start these particular exercises.
Side effects and possible complications
Some of the side effects and possible complications of hysterectomy include:
- Nausea and vomiting.
- Infection.
- Internal haemorrhage.
- Build-up of blood beneath the stitches.
- Internal scar tissue.
- Allergic reaction to the anaesthetic.
- Blood clots.
- Vaginal vault prolapse.
- Feelings of grief and loss.
- Injury to the bowel, bladder or ureters (tubes that carry urine from the kidneys to the bladder) - this is rare.
- Fistula (abnormal hole between internal structures, such as the bowel and vagina). This is also rare.
Taking care of yourself at home
Be guided by your doctor, but general suggestions for the six week post-operative period include:
- REST - try to rest as much as possible for at least two weeks. You should avoid driving during this time.
- EXERCISE- continue with the exercises you were shown in hospital. After two weeks of rest, you should aim to go for a 10 minute walk each day, unless advised otherwise by your doctor.
- STANDING - avoid standing for more than a few minutes at a time in the early post-operative period. You can increase standing time as recovery progresses.
- LIFTING- avoid heavy lifting and stretching.
- CONSTIPATION - to avoid constipation, drink plenty of fluids and eat fresh fruits and vegetables. You may wish to take stool softeners for the first few days.
- MEDICATION - if you have been prescribed antibiotics, make sure you take the full course, even if you feel well.
- SEX - it is advised that you avoid penetrative sex until after the post-operative check (at about six weeks) to ensure the vagina is fully healed. If vaginal dryness is a problem, it may be helpful to use a water based lubricant.
Long term outlook
After hysterectomy, you will no longer need contraception or have menstrual periods. If your ovaries were removed, you will experience sudden menopause. You may want to discuss short term hormone replacement therapy (HRT) or other options with your doctor. Hysterectomy can be effective for gynaecological complaints like fibroids and endometriosis, but some conditions (such as cancer) may recur. You will need to have regular check-ups to make sure you are cancer free. You may need to have a regular vault smear. This test is similar to a Pap smear but it takes cells from the vaginal walls instead of the cervix.
Other forms of treatment
Many of the various gynaecological conditions cured by hysterectomy can often be successfully treated using other methods, including:
- FIBROID- options include surgery to remove the fibroids (myomectomy), drugs to temporarily block the action of sex hormones and shrink the growths, or else the fibroids can be frozen, cauterised or removed by laser (myolysis).
- HEAVY BLEEDING - options include taking the contraceptive pill to regulate the periods, other hormonal drug therapies, surgical removal of the endometrium, or the insertion of an intrauterine device (IUD) that releases small amounts of synthesised sex hormone into the uterus.
- UTERINE PROLAPSE- options include pelvic floor exercises, the insertion of a ring-shaped pessary into the vagina to prop up the uterus, or surgical repair.
- ENDOMETRIOSIS - options include hormonal drugs, surgical removal of the endometrium, or the insertion of an intrauterine device (IUD) that releases small amounts of synthesised sex hormone into the uterus.
- Hysterectomy is the surgical removal of the uterus.
- A hysterectomy may be performed to correct various gynaecological problems including abnormal menstrual bleeding, fibroids, endometriosis, and cancer of the uterus, ovary or cervix.
- The operation may be performed via an abdominal incision or through the vagina.
- Apart from cancer, many of the various gynaecological conditions cured by hysterectomy can often be successfully treated using other methods
Things to remember
Labels: Carcinoma, Gynecology, Myoma Uteri, Uterine Bleeding
Hysterectomy is the surgical removal of the womb (uterus), with or without the removal of the ovaries.
The uterus is a muscular organ of the female body, shaped like an inverted pear.
The lining of the uterus, the endometrium, thickens during ovulation in preparation for receiving a fertilised ovum. If the ovum is unfertilised, the lining comes away. This is known as menstruation. If the ovum is fertilised, the developing baby is nurtured inside the uterus throughout the nine months of pregnancy.
Once a hysterectomy is performed, a woman can no longer have children or menstrual periods. Hysterectomy is used to treat a number of conditions, such as excessive menstrual bleeding.
There are concerns that more hysterectomies are performed than are necessary.
Reasons for hysterectomy
The conditions that may be treated by hysterectomy include:
- FIBROIDS , which are non-malignant growths inside the muscular walls of the uterus.
- Heavy or irregular menstrual periods or MENORRHAGIA
- Severe period pain, or DYSMENORRHOEA.
- CANCER of the cervix, uterus or ovaries.
- ENDOMETRIOSIS , a condition characterised by the migration of cells from the lining the uterus to other areas of the body.
- PROLAPSE, which means the uterus falls into the vagina because of loose ligaments or damage to the pelvic floor muscles.
- PELVIC INFLAMATORY DISEASE , caused by bacterial infection.
Degrees of hysterectomy
There are three basic types of hysterectomy:
- TOTAL HYSTERECTOMY - removal of the uterus and cervix. The ovaries and tubes remain.
- SUBTOTAL HYSTERECTOMY - removal of the body of the uterus. The cervix, ovaries and the tubes remain.
- TOTAL HYSTERECTOMYY and BILATERAL SALPHYNGO OOPHORECTOMY - removal of the uterus, cervix, ovaries and tubes.
Different surgical procedures
The type of procedure used influences the length of hospital stay and recovery time. Hysterectomy procedures include:
- VAGINAL - the uterus is removed through an incision in the top-end of the vagina. There are no cuts to the abdomen.
- VAGINAL and LAPAROSCOPY - an instrument called a laparoscope is inserted through small abdominal incisions to assist in the vaginal removal of the uterus. During laparoscopic-assisted vaginal hysterectomy, surgery is performed through three to four small incisions in the abdomen and completed through the vagina.
- ABDOMINAL - the uterus is removed through a lower abdominal incision. With a total abdominal hysterectomy, surgery is performed through a long abdominal cut similar to that which is conducted for a caesarian section.
Possible complications
Possible complications of hysterectomy include:
- Difficulties with urination
- Decreased sexual desire
- Constant pelvic pain
- Psychological distress
- Complications of any operation or anaesthetic.
Women of childbearing age
Once a hysterectomy of any kind is performed, pregnancy is no longer possible.
If the ovaries of a premenopausal woman are removed, then ovulation will also cease. This means there will be a drop in production of the sex hormones oestrogen and progesterone, which can cause vaginal dryness, hot flushes, sweating and other associated symptoms of natural menopause.
Women who undergo bilateral oophorectomy, or removal of both ovaries, are usually treated with hormone replacement therapy (HRT) - also known as hormone therapy (HT) - to maintain their hormone levels.
The other roles of the uterus and ovaries
Once the childbearing years are finished, hysterectomy may seem a logical treatment option. This is because pregnancy is often considered to be the only function of the uterus, which may explain Australian's high hysterectomy rate. However, the uterus has a number of other important functions, including:
- SEXUALLITY- the uterus rhythmically contracts during orgasm, contributing to sensations of pleasure.
- HORMONE PRODUCTION - some researchers believe the uterus contributes to the maintenance of the female hormonal system. The ovaries also play a major role in maintaining the female hormonal system. Their removal results in instant menopausal symptoms and therefore, unless diseased, they should not be removed during hysterectomy.
- SELF IMAGE - the uterus is of considerable psychological importance, whether or not it is menstruating and capable of bearing a child.
Other treatments
The conditions that prompt a hysterectomy can often be treated by other means. It is recommended that women consider hysterectomy as a procedure of last resort, when all other treatment options have failed. Other options include:
- DRUG TREATMENT - medications may be given to reduce or stop heavy bleeding. This is generally used in the short term to provide symptom relief and to allow women time to explore and consider other treatment options.
- ENDOMETRIAL ABLATION - this involves the removal or stripping of the lining of the uterus, which is shed each month as a period. This procedure requires admission to hospital as a day patient. An anaesthetic is used. Endometrial ablation can successfully reduce or stop heavy bleeding in 85 per cent of cases. It is not recommended for women who wish to become pregnant.
- CONSERVATIVE TREATMENT OF FIBROID - the size, number and position of the fibroids will determine the treatment options offered. Fibroids can be 'shrunk' using medication or by surgery, which burns them away. They can also be starved of a blood supply required for growth, or they can be individually removed through surgery, leaving the uterus intact. Sometimes a combination of these treatments may be advised.
- SURGICAL REMOVAL OF ENDOMETRIOSIS - this involves cutting or burning out tissue deposits and adhesions from such areas as the ovaries, bladder, bowel, uterus, pelvic walls and ligaments which support the uterus. Hormone therapy may be used before or after surgery.
- REMOVAL OF ADENOMYOSIS - localised disease can be excised (cut out) or diathermied (burnt off), leaving the uterus intact. This procedure is recommended for those women who wish to become pregnant. It has a 50 per cent success rate - that is, adenomyosis recurs in approximately one half of cases.
Things to remember
- Hysterectomy is the surgical removal of the womb (uterus), with or without the removal of the ovaries.
- Hysterectomy is used to treat a variety of conditions, including heavy or painful periods, fibroids and prolapse.
- It is recommended that women consider hysterectomy as a procedure of last resort, when all other treatment options have failed.
Labels: Carcinoma, Gynecology, Myoma Uteri, Uterine Bleeding
A myomectomy is an operation performed to remove benign tumours called fibroids from the muscular wall of the uterus.
Fibroids often cause pain and excessive menstrual bleeding. They can also interfere with your ability to become pregnant. They may degenerate or become infected, and therefore your doctor may feel they should be surgically removed.
A hysterectomy may be suggested if you are over childbearing age.
Uterine fibroids
Fibroids are categorised by their locations, which include:
- INTRAMURAL- in the uterine wall. Intramural fibroids are the most common variety.
- SUBMUCOSAL - in the uterine lining (endometrium). This type tends to cause excessive menstrual bleeding and period pain.
- SUBSEROSAL- on the exterior wall of the uterus. They sometimes appear like long stalks.
Medical issues to consider
Your doctor may order an ULTRASOUND SCAN to try to pinpoint the fibroids prior to surgery.
Some BLOOD TESTS may be ordered to see if you are anaemic (symptoms can include excessive tiredness, breathlessness on exertion, pale skin and poor resistance to infection).
A URINE TEST will tell if you have an infection in your urinary system.
The ANAESTHETIST VISITS anaesthetist visits you prior to your operation to see if you are suitable to have a general anaesthetic. (If you are not suitable, you may have the operation performed under a spinal or epidural anaesthetic.) For a general anaesthetic, you are usually given a pre-medication injection to dry up your internal secretions and make you feel drowsy.
Some surgeons request you have an ENEMA and a portion of your pubic hair shaved prior to surgery.
Operation procedure
In most cases, the surgeon performs a DILATATION and CURETTAGE (D&C) to check for irregularities in the inner surface of the uterus. The kind of myomectomy performed depends on the type, size, number and location of the fibroids, but can include:
- ABDOMINAL MYOMECTOMY - the uterus is accessed via one large incision through the abdomen. Usually, a horizontal cut just on the bikini line is performed; in some cases, the incision may need to be made vertically in the midline of your abdomen. The uterus is cut, sometimes with a laser (which closes off blood vessels and reduces bleeding). The fibroids are then removed and the uterus, abdominal wall and skin are closed with sutures. This type of myomectomy is preferred for multiple or deeply rooted fibroids. The drawback of abdominal myomectomy is that it takes longer to recover.
- LAPAROSCOPIC MYOMECTOMY - subserosal fibroids can often be removed via laparoscopic (‘keyhole’) myomectomy. The surgeon makes a number of small incisions, which allow different instruments access to the uterus. Among these instruments is the laparoscope, which contains fibre-optic camera heads or surgical heads (or both). The fibroids are removed, and the small wounds sutured (sewn) closed. Recovery time for the patient is comparatively fast.
- HYSTEROSCOPIC MYOMECTOMY - the fibroids are removed via the dilated cervix, so no abdominal incisions are needed. The instrument is called a resectoscope, which is a hysteroscope fitted with a wire loop. The instrument is inserted through the cervix, and the wire loop slung over the fibroid. Electrical energy passes through the loop, which cuts the fibroid loose. The fibroid can then be removed through the vagina.
| | |
Immediately after the operation
After the operation, you can expect:
- Your temperature, pulse, respiration and blood pressure is observed and noted.
- Any vaginal discharge is noted.
- An intravenous fluid line may still be running into your arm to replace fluids in your body. Antibiotics may be included to combat infection.
- You may have some tubes at the wound site to drain off excess fluid if necessary.
- If you need pain relief, tell your nurse.
- You may have a catheter to drain off urine for the next day or so.
- You are given a normal diet, once your doctor feels it is safe to do so. Tell your nurses as soon as you pass wind or a bowel motion, as this shows that your digestive system is getting back to normal.
- Perform your breathing, coughing and leg exercises hourly when you are awake.
- You are assisted out of bed and taken for a walk the day following surgery.
- You may be in hospital for five to seven days following surgery.
Possible complications
Possible complications of myomectomy include:
- Haemorrhage
- Injury to the uterus
- Damage to the nearby organs of the urinary system
- Formation of scar tissue (adhesions) within the uterus
- Infection
- Blood clots
- Eventual re-growth of fibroids.
Taking care of yourself at home
Be guided by your doctor, but general suggestions include:
- TRY TO REST as much as possible for two weeks.
- Avoid standing for more than a few minutes at a time.
- Continue to TAKE YOUR MEDICATION , and follow strictly the instructions on taking your antibiotics.
- After two weeks, AIM TO WALK for about 10 minutes every day, unless advised otherwise by your doctor.
- Depending on the type of surgery, you can RETURN TO WORK rk within two to six weeks (abdominal myomectomy takes the longest recovery time).
- If you have any excessive vaginal bleeding, or signs of infection at your wound site (such as redness, increasing pain, swelling, or an increased or offensive discharge from your wound), see your doctor immediately.
Long term outlook
You will still have your uterus and all reproductive organs following myomectomy.
Once healed, there should be no effects on your sexual activity, and you should still be able to conceive. Depending on the depth of the scar in your uterus, you may require an elective caesarean section at 38 weeks to safely give birth.
If you are seeking myomectomy as a remedy to excessive menstrual bleeding, it is important to know that the operation is unsuccessful in around 20 per cent of cases - your heavy menstrual flow may be due to factors other than fibroids. See your doctor for further information and advice.
Other forms of treatment
Other possible forms of treatment for fibroids may include:
- MONITORING - if the fibroids are asymptomatic, a ‘wait and see’ approach is often adopted.
- DRUGS - such as hormones, used in combination, to shrink the fibroids prior to surgery.
- HYSTERECTOMY- the surgical removal of some or all of the uterus. Pregnancy is no longer possible after a hysterectomy.
Labels: Gynecology, Myoma Uteri, Uterine Bleeding
UTERINE MYOMA
Fibroids, or myomas, are growths or benign tumours that form inside the uterus (womb). Around four in 10 women over the age of 40 will have fibroids.
No one knows why fibroids develop, but it is suspected that the sex hormones – oestrogen and progesterone – play significant roles. This is because fibroids rarely grow in prepubescent girls and postmenopausal women.
Pre-existing fibroids stop growing, and may even shrink, once a woman passes the menopause.
Fibroids often cause no problems, but may occasionally be associated with infertility, miscarriage and premature labour. Other possible problems include heavy, lengthy and painful periods. Treatment depends on the size, number and location of the fibroids, but may include drugs, procedures performed under local anaesthetic and surgery. Fibroids rarely turn cancerous.
Symptoms
Most women with fibroids have no symptoms. When present, symptoms may include:
- Heavy periods
- Lengthy periods
- Period pain
- Spotting between periods
- Painful intercourse
- A sensation of heaviness or pressure in the back, bowel and bladder
- Frequent urination
- A lump or swelling in the lower abdomen.
Different types
Fibroids are categorised by their location, which includes:
- INTRAMURAL – growing in the uterine wall. Intramural fibroids are the most common variety.
- SUBMUCOSAL– growing in the uterine lining (endometrium). This type tends to cause excessive menstrual bleeding and period pain.
- SUBSEROSAL – growing on the exterior wall of the uterus. These sometimes appear like long stalks.
Common complications
Fibroids can cause a variety of complications, including:
- ANEMIA – excessive menstrual blood loss can cause anaemia, a disorder characterised by the body’s inability to carry sufficient oxygen in the blood. Symptoms of anaemia include breathlessness, fatigue and paleness.
- URINATION PROBLEMS– large fibroids can bulge the uterus against the bladder, causing a sensation of fullness or discomfort and the need to urinate often.
- INFERTILITY – the presence of fibroids can interfere with implantation of the fertilised egg in a number of ways. For example, the egg may try to burrow into a fibroid, or fibroids close to the uterine cavity may ‘prop open’ the uterus, making successful implantation difficult.
- MISCARRIAGE and PREMATURE DELIVERY – fibroids can reduce blood flow to the placenta or may compete for space with the developing baby.
Diagnosis
Uterine fibroid (right lateral wall)
Nine (9) weeks and 4 days gestation
Fibroids can be detected using an ULTRASOUND , where sound waves create a two-dimensional picture.
The inside of the uterus can be examined with a HYSTEROSCOPE , which is a thin tube passed through the cervix (neck of the womb). A small camera may be placed at the tip of the hysteroscope, so that the interior of the uterus can be viewed on a monitor.
Treatment
Treatment depends on the location, size and number of the fibroids, but may include:
- MONITORING – if the fibroids are causing no symptoms and are not large, a ‘wait and see’ approach is usually adopted.
- DRUGS– such as hormones, used in combination to shrink the fibroids prior to surgery.
- ARTERIAL EMBOLISATION – under local anaesthetic, a fine tube is passed via an artery in the arm or leg into the main artery supplying the fibroid with blood. The whole process is monitored by x-ray. Fine particles (like sand) are then injected into the artery to block the blood supply to the fibroid. The fibroid slowly dies and symptoms should settle over a few months.
- HYSTEROSCOPY – the fibroids are removed via the cervix, using a hysteroscope.
- LAPAROSCOPY – or ‘keyhole surgery’, where a thin tube is inserted through the abdomen to remove the fibroids.
- OPEN SURGERY– larger fibroids need to be removed via an abdominal incision. This procedure weakens the uterine wall and makes Caesarean sections for subsequent pregnancies more likely.
- HYSTERECTOMY – the surgical removal of some, or all, of the uterus. Pregnancy is no longer possible after a hysterectomy.
Labels: Gynecology, Uterine Bleeding
Visitor
Labels
- Carcinoma (2)
- Dysmenorrhoea (4)
- Endometriosis (4)
- Female Genital Infection (3)
- Fluor Albus (4)
- General (3)
- Genital Prolapse (4)
- Gynecology (8)
- Infectious Disease in Pregnancy (13)
- Infertility (10)
- Menopause (3)
- Menstrual Disorder (10)
- Myoma Uteri (3)
- Obstetrics (13)
- Pelvic Floor (4)
- Pelvic Inflamatory Disease (3)
- Physiology of Human Reproductive System (4)
- Pregnancy (2)
- Sexually Transmitted Disease (6)
- Uterine Bleeding (4)
Followers
Facebook Badge
Copyright © 2009 Complicated Girl. All Rights Reserved.