Information Site About Reproductive System
About Me
Blog Archive
-
▼
2009
(58)
-
▼
December
(17)
- Syphilis During Pregnancy
- STDs and Pregnancy - Fact Sheet
- URINARY TRACT INFECTIONS in PREGNANCY
- GROUP B STREPTOCOCCUS INFECTION and PREGNANCY
- SWINE FLU and PREGNANCY
- GENITAL HERPES IN PREGNANCY
- LISTERIA and PREGNANCY
- REPIRATORY INFECTIONS DURING PREGNANCY
- HEPATITIS IN PREGNANCY
- CYTOMEGALOVIRUS
- CHLAMYDIA
- RUBELLA
- TOXOPLASMOSIS
- RECTOCELE
- CYSTOCELE
- PROLAPSE OF THE UTERUS
- PELVIC FLOOR
-
▼
December
(17)
Sunday, November 29, 2009
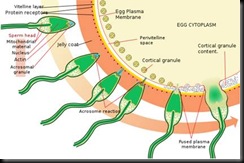
The acrosome reaction for a sea urchin, a similar process. Note that the picture shows several stages of one and the same spermatozoon - only one penetrates the ovum
Human fertilization is the union of a human egg and sperm, usually occurring in the ampulla of the uterine tube. It is also the initiation of prenatal development. Scientists discovered the dynamics of human fertilization in the nineteenth century.[1]
Fertilization (also known as conception, fecundation and syngamy), is the fusion of gametes to produce a new organism. The process involves a sperm fusing with an ovum, which eventually leads to the development of an embryo.
It is when first of all the acrosome at the head tip produces enzymes, which cuts through the outer jelly coat of the egg. After that has happened, the sperm plasma fuses with the egg’s plasma membrane. Finally, the Head disconnects with the body, and the egg can now travel down the Fallopian tube to reach the womb, where the baby grows.
Fertilization may or may not involve sexual intercourse. In vitro fertilisation (IVF) is a process by which egg cells are fertilized by sperm outside the womb, in vitro. Sperm is propelled through the female reproductive tract by flagellation and may get through the jelly coat through a process called sperm activation. The oocyte and sperm fuse once the sperm is through the corona radiata and the zona pellucida; two layers covering and protecting the oocyte from fertilization by more than one sperm.
Corona radiata
Human ovum examined fresh in the liquor folliculi. The zona pellucida is seen as a thick clear girdle surrounded by the cells of the corona radiata.
The egg itself shows a central granular deutoplasmic area and a peripheral clear layer, and encloses the germinal vesicle, in which is seen the germinal spot.
The egg binds the sperm through the corona radiata, a layer of follicle cells on the outside of the secondary oocyte. Fertilization is when the nuclei of a sperm and an egg fuse. The successful fusion of gametes form a new organism.
Acrosome reaction
The acrosome reaction must occur to mobilise enzymes within the head of the spermatozoon to degrade the zona pellucida.
Zona pellucida
The sperm then reaches the zona pellucida, which is an extra-cellular matrix of glycoproteins. A special complementary molecule on the surface of the sperm head then binds to a ZP2 glycoprotein in the zona pellucida. This binding triggers the acrosome to burst, releasing enzymes that help the sperm get through the zona pellucida.
Some sperm cells consume their acrosome prematurely on the surface of the egg cell, facilitating for other surrounding sperm cells, having on average 50% genome similarity, to penetrate the egg cell.[2] It may be regarded as a mechanism of kin selection.
Recent studies have shown that the egg is not passive during this process.[3][4]
Cortical reaction
Once the sperm cells find their way past the zona pellucida, the cortical reaction occurs: cortical granules inside the secondary oocyte fuse with the plasma membrane of the cell, causing enzymes inside these granules to be expelled by exocytosis to the zona pellucida. This in turn causes the glyco-proteins in the zona pellucida to cross-link with each other, making the whole matrix hard and impermeable to sperm. This prevents fertilization of an egg by more than one sperm.
Fusion
After the sperm enters the cytoplasm of the oocyte, the cortical reaction takes place, preventing other sperm from fertilizing the same egg. The oocyte now undergoes its second meiotic division producing the haploid ovum and releasing a polar body. The sperm nucleus then fuses with the ovum, enabling fusion of their genetic material.
Cell membranes
The cell membranes of the secondary oocyte and sperm fuse together.
Transformations
Both the oocyte and the sperm go through transformations, as a reaction to the fusion of cell membranes, preparing for the fusion of their genetic material.
The oocyte now completes its second meiotic division. This results in a mature ovum. The nucleus of the oocyte is called a pronucleus in this process, to distinguish it from the nuclei that are the result of fertilization.
The sperm's tail and mitochondria degenerate with the formation of the male pronucleus. This is why all mitochondria in humans are of maternal origin.
Replication
The pronuclei migrate toward the center of the oocyte, rapidly replicating their DNA as they do so to prepare the new human for its first mitotic division.
Mitosis
The male and female pronuclei don't fuse, although their genetic material do so. Instead, their membranes dissolve, leaving no barriers between the male and female chromosomes. During this dissolution, a mitotic spindle forms around them to catch the chromosomes before they get lost in the egg cytoplasm. By subsequently performing a mitosis (which includes pulling of chromatids towards centrioles in anaphase) the cell gathers genetic material from the male and female together. Thus, the first mitosis of the union of sperm and oocyte is the actual fusion of their chromosomes.
Each of the two daughter cells resulting from that mitosis have one replica of each chromatid that was replicated in the previous stage. Thus, they are genetically identical.
In other words, the sperm and oocyte don't fuse into one cell, but into two identical cells.
Footnotes
- ^ Garrison, Fielding. An Introduction to the History of Medicine, pages 566-567 (Saunders 1921).
- ^ Sleek, Fast and Focused: The Cells That Make Dad Dad New York Times 2007/06/12
- ^ Suzanne Wymelenberg, Science and Babies, National Academy Press, page 17
- ^ Richard E. Jones and Kristin H. Lopez, Human Reproductive Biology, Third Edition, Elsevier, 2006, page 238
Sunday, October 25, 2009
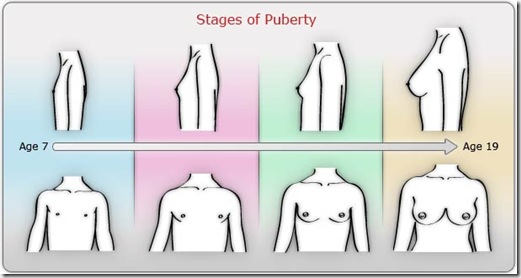
Puberty is the time in our lives when our sexual and reproductive organs mature. This means our bodies become capable of creating babies. Long before any outward changes happen, special hormones begin to be produced inside the bodies of both girls and boys. These hormones affect many different things, including sexual development and growth.
Puberty starts around 11 years for girls and 12 years for boys, give or take a year or so. Physical changes become obvious at about 11 to 14 years for most girls, and about 13 to 16 years for most boys. Along with these physical changes come emotional changes. We also start to think differently at this time in our lives. There are quite a few major changes to deal with during puberty.
Physical changes for girls
If you’re a girl, the physical changes you’ll notice around puberty include:
- Height – you’ll grow taller.
- Curves develop – your hips widen and your body is becoming curvier.
- Breasts begin to form – the first stage is called ‘budding’. Sometimes your breasts may be different sizes. This is normal. If you’re worried, see a doctor or other health professional.
- Hair growth – hair will start to grow around the pubic area and underarms, while hair on the legs and arms darkens.
- Vaginal discharge – you may start to get a whitish discharge from the vagina. This is a natural self-cleaning process the vagina uses and it’s nothing to worry about.
- Periods – your menstrual periods start. The bleeding from your period is not like bleeding from injury; it’s a normal process where the body removes the lining of the uterus (womb) that has built up over the last month.
- Period pain – You may start to have period pain just before, or at the beginning of, a period. Warm drinks and a hot water bottle (held to the tummy) can be helpful. For some women, exercise helps. See a doctor if you have too much pain. Sometimes, medication is needed.
Menstrual periods
You can’t tell for sure exactly when you’ll get your period. Usually your period will start off lightly, so you will have plenty of time to get to the bathroom. You may notice you feel damp or wet.
Some women get period pain or cramp in the lower abdomen (tummy) that tells them that they’ll get their period soon. You may notice a slight clear or whitish discharge between periods, before you get your first period, or both.
Periods can be irregular, especially at first. They may vary both in how often they happen and how long they last. After the first year or so, periods tend to become fairly regular; usually they come about once every four weeks.
Pads and tampons
Carry a sanitary pad or tampon in your purse or school bag to be prepared. A pad is usually the easiest to use at first. Change pads and tampons regularly, at least two or three times a day, depending on the menstrual flow.
It’s important to make sure that the vagina does not get too dry, so you may need to use smaller tampons or a pad when your flow is light. Tampons have been associated with toxic shock syndrome (a very serious illness) when not changed regularly.
Physical changes for boys
If you’re a boy, the physical changes you’ll notice around puberty include:
- Height and muscles – you’ll get taller and stronger and start to develop muscle mass.
- Genitals – your testicles and penis size increase. It’s normal for one testicle to be bigger than the other. Some young men worry about their penis size; however, sexual functioning – including the ability to have sexual intercourse and father children – doesn’t depend on penis size. If you’re worried, have a chat to a doctor or health professional.
- Hair growth – body hair begins to grow around the pubic area, legs, underarms and on the face. The hair starts off fine and becomes coarser and darker over the years of puberty. Some men continue to grow a bit and develop more body hair right into their 20s.
- Voice changes – in puberty, the voice becomes deeper. This is sometimes called ‘voice breaking’ because of the ups and downs in tone.
- Wet dreams – nocturnal emissions, or wet dreams, can happen in your sleep. Wet dreams are an ejaculation of semen – not urine – that has dampened your sheets. This is a normal part of growing up.
- Erections – sometimes erections can happen because you’re nervous or excited, or just for no reason at all, and can make you feel embarrassed. Other people usually don’t notice them as much as you do and they go away within minutes.
- Breast changes – some boys’ breasts may grow slightly or feel tender. This is a normal reaction to the hormones in your body. This will eventually go away.
Although puberty refers to the physical changes of the body, there are also many emotional changes taking place, which affect boys and girls. They include:
- Coping with your changing body – young people have to deal with rapid physical change; all of a sudden, you have a new body shape and you may begin to feel self-conscious about how you look. You might feel embarrassed if you feel different to your friends. Other people may start to respond to you differently. You look older and may be treated as an older person.
- Frustration because you feel different – it can be difficult to cope with early physical changes or it also can be frustrating waiting for physical changes to happen.
- Mood swings – the rapid and abrupt release of hormones into your body can bring about extremes in emotion and mood. It’s a temporary imbalance and will settle down. Your parents might complain about your moods, but remember … it’s not the real you. It’s just those wild hormones affecting the way you feel.
- Energy changes – the fast physical growth and other changes in your body can mean you swing between having boundless energy and being extremely tired.
Your thinking will change
The way you think changes around this time. You’re starting to choose your own standards and ideals; to form your own ideas, morals and values; and to rely less on your parents for knowledge about life and the world. You may be starting to think about some deep questions like ‘Who am I?’, ‘Why am I here?’ or ‘What is the meaning of life?’.
You’re developing your own identity as an individual rather than as a part of the family. This could mean showing your parents or the world that you have very different individual tastes in your personal style. Some young people choose to do this in wild ways, while others take a more subtle approach.
Your relationship with your parents
You may want more independence, while – on the other hand – not wanting to give up the support of your parents just yet. This can mean that one minute you feel quite adult and the next you’re feeling like a child again. It may mean that you act impulsively at times and engage in some risk-taking behaviour.
Parents sometimes worry a lot when you want to go out on your own and do things independently, because they don’t want you to come to any harm. They may either know first hand or have heard of some people who take advantage of young people. They’re probably quite aware of the risks that some young people take (they may have done it themselves).
What this means is that there can be conflict between parents (who want their child safe) and a young person who wants independence. Try to sit down and work it out calmly with your parents.
Getting through puberty
Puberty can be an unsettling time. It can also be an exciting time, as you move from childhood to adulthood, and take on all the rights and responsibilities of adulthood. Puberty can be difficult for parents and for young people as everyone adjusts to the changes. Everyone needs to have patience.
Parents are learning too. If there are disagreements, listen to what they have to say and let them know your point of view. Show them that you can take care of yourself in a mature and wise fashion.
Try to be considerate – for example, let your parents know where you are and if you have a change of plans. These small things can make a huge difference. They will show your parents that you can act responsibly and safely.
By handling situations calmly and maturely, your parents will build up their trust in you and come to realise you are on the way to being able to take care of yourself!
Things to remember
- Puberty is the time in our lives when our sexual and reproductive organs mature.
- Although puberty refers to the physical changes of the body, there are also many emotional changes.
- Puberty can be difficult for parents and for young people, as everyone adjusts to the changes.
Saturday, October 24, 2009

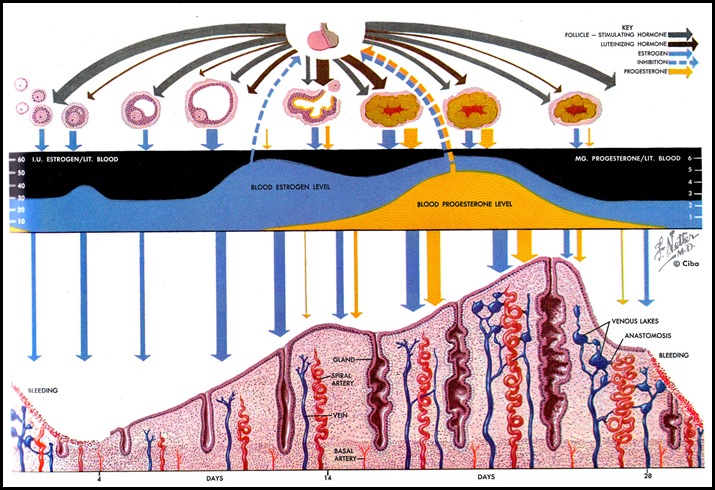
New life begins if the ovum meets with a sperm during its journey down the fallopian tube.
Ovulation depends on a complex interplay of glands and their hormones, and generally occurs about 2 weeks before the onset of the menstrual period.
Typical ovulation symptoms and signs include changes in cervical mucus and a small rise in basal temperature. For most women, ovulation occurs about once every month until menopause, apart from episodes of pregnancy and breastfeeding. However, some women experience irregular ovulation or no ovulation at all.
Signs of ovulation
The female body shows several signs of ovulation. You may experience some or all of these signs, including:
- Regular menstrual cycles - menstrual periods that arrive every 24-35 days are more likely to be ovulatory than periods that occur more or less often.
- Mucus changes - about two weeks before menstruation, an ovulating woman may notice slick and slippery mucus.
- Abdominal pain - some women experience pain during ovulation. The pain may be general or localised to one side of the abdomen.
- Premenstrual symptoms - ovulation may accompany premenstrual symptoms such as breast enlargement and tenderness, abdominal bloating and moodiness.
- Temperature rise - women who use a natural family planning method of contraception will notice a small rise in their basal temperature after ovulation has occurred. The temperature rise is about half a degree Celsius. This temperature rise does not predict ovulation - it suggests that ovulation has already taken place.
Ovulation depends on the activity of various structures and their hormones, including:
- Hypothalamus - located within the brain. The hypothalamus uses hormones to communicate with the pituitary.
- Pituitary - known as the ‘master gland’ of the hormone (endocrine) system. It is located within the brain, at the base of the skull, and is connected to the hypothalamus by a thin stalk. It uses chemicals to prompt the ovaries to produce their hormones.
- Ovaries - the two almond-shaped glands located within a woman’s pelvis that contain the ova. The ovaries make the two female sex hormones oestrogen and progesterone.
Ovulation is part of the menstrual cycle. This cycle is caused by the complex and interrelated activity of various hormones. The cycle includes:
- Menstruation - the shedding of the uterine lining.
- Follicular phase - the hypothalamus triggers the pituitary gland to release follicle stimulating hormone (FSH), which prompts the ovaries to produce up to 20 follicles. Each follicle contains an immature ovum. Usually, only one follicle survives to maturity. Assuming the menstrual cycle is around 28 days long, a single ovum matures at about day 10. This event also prompts the thickening of the uterine lining (endometrium) in preparation for a fertilised ovum.
- Ovulation - the maturing follicle prompts the release of higher amounts of oestrogen. The hypothalamus responds by secreting a chemical known as gonadotrophin-releasing hormone (GnRH), which makes the pituitary produce luteinising hormone (LH) and FSH. High levels of LH trigger ovulation within about two days. The mature follicle releases the ovum into the peritoneal cavity; it is then drawn into the open end of the fallopian tube. Small hair-like structures within the fallopian tube wave or ‘massage’ the ovum towards the uterus. Unless the ovum encounters a sperm within 24 hours, it will die.
- Luteal phase - the follicle becomes the corpus luteum, a structure that makes the hormone progesterone. Unless a fertilised ovum implants into the uterine lining, the corpus luteum dies. Without its contribution of progesterone, the uterus can’t maintain the thickened uterine lining, and menstruation occurs. ( picture below )
Ovulation predictor kits
There are many different kinds of ovulation predictor kits on the market. Most work by measuring the level of luteinising hormone (LH) in the woman’s urine. LH levels rise about 24 to 36 hours before ovulation takes place. You need to estimate your approximate time of ovulation if you’re to use these kits effectively. All kits come with detailed instructions and a number of testers, but one way to calculate your estimated time of ovulation includes:
- Work out the length of your average menstrual cycle. Day one is the first day of the menstrual period and the last day is the day before the next period begins. Let’s say the menstrual cycle is 28 days long.
- Subtract 17 days. In our example, 28 days minus 17 days equals day 11.
- Use the ovulation predictor kit on day 11. Continue testing daily until the test comes back positive. A positive result means you are going to ovulate within the next 24 to 36 hours.
- Having sex around the time of ovulation means that the sperm and ovum have a good chance of meeting in the fallopian tube.
Medical tests can check whether or not ovulation took place. These tests can include:
- Blood test - to check for the presence of progesterone. A level greater than 20nmol/L indicates that ovulation took place. This test must be taken about three to 10 days before the first day of the next expected period.
- Pregnancy ultrasound - the presence of a foetus is the only 100 per cent proof that ovulation took place. Medical tests such as ovulation predictor kits and blood tests can only ascertain that ovulation probably - not definitely - occurred.
Common causes of ovulatory problems include:
- Hypothalamus - events that can alter the functioning of the hypothalamus include polycystic ovary syndrome, overexercising, poor nutrition and chronic stress.
- Pituitary - events that can prevent the pituitary gland from producing enough hormones include benign pituitary tumours or direct injury to the pituitary itself.
- Ovary - events that can prevent the ovaries from releasing ova include early menopause (also known as ovarian failure), or damage to or removal of the ovaries.
Ways to increase your chances of ovulation include:
- Women who are seriously obese or underweight may have problems with ovulation. Try to keep your weight around the average for your height and build.
- Excessive exercise can prevent ovulation. Ease back on your physical activity levels - this may require expert help if your desire to exercise is actually a form of bulimia.
- Repeated crash dieting, fasting, skipping meals and other disordered eating habits can hamper your body’s ability to regularly ovulate. Make sure to eat properly and regularly. Once again, you may need expert help if these habits are associated with an eating disorder such as anorexia or bulimia nervosa.
- Chronic emotional stress can play havoc with your menstrual cycle. Try to reduce the amount of stress in your life, and learn ways to better cope with stress. For example, relaxation training may be helpful.
Some women who aren’t ovulating regularly can be helped by reproductive technologies including tablets and injections to trigger higher production of ovulatory hormones. The dosage needs to be carefully monitored, because ovulation induction can trigger the maturation of a number of ova, which could lead to multiple pregnancies.
The average length of the menstrual cycle is 28 days, although this can vary between women, and from one cycle to the next in individuals. The length of the menstrual cycle is calculated from the first day of the period to the day before the next period begins. Menarche (the onset of the first period) occurs, on average, between the ages of 11 and 14 years. Usually, the young woman has already developed secondary sexual characteristics, such as pubic hair and budding breasts.
Hormones and the menstrual cycle
The menstrual cycle is complex, controlled by a variety of glands and their associated hormones. A brain structure called the hypothalamus influences the nearby pituitary gland to secrete special chemicals, which prompt the ovaries to secrete their sex hormones, principally oestrogen and progesterone. The menstrual cycle is a biofeedback system, which means all of the structures and glands are influenced by the activity of the others. There are four main phases of the menstrual cycle: menstruation, the follicular phase, ovulation and the luteal phase.
Menstruation
This is the elimination of the thickened uterine lining from the body via the vagina. Menstrual fluid contains blood, cells from the uterine lining (endometrial cells) and mucus. The average length of a period is between three days and one week, depending on the individual. Sanitary pads or tampons are used to absorb the menstrual flow. Both pads and tampons need to be changed regularly, at least every four hours. Tampon use has been associated with an increased risk of a particularly rare illness called toxic shock syndrome.
Follicular phase
The follicular phase spans the length of time between the first day of menstruation and the moment of ovulation. Prompted by the hypothalamus, the pituitary gland releases follicle stimulating hormone (FSH). This hormone stimulates the ovary to produce around five to 20 follicles (tiny nodules or cysts), which bead on the surface. Each follicle houses an immature egg. Typically, only one follicle will mature into an egg, while the others die away. This can occur at around day 10 of a 28-day cycle. The growth of the follicles stimulates the lining of the uterus (endometrium) to thicken in preparation for possible pregnancy.
Ovulation
Ovulation means the release of a mature egg from the ovary surface. This occurs roughly at mid-cycle, around two weeks or so before the onset of menstruation. During the follicular phase, the ripening follicle causes a rise in the level of the sex hormone oestrogen. The hypothalamus in the brain recognises these rising levels and releases a chemical called gonadotrophin-releasing hormone (GnRH). This hormone prompts the nearby pituitary gland to produce boosted levels of luteinising hormone (LH) and FSH. Within two days, ovulation is triggered by the high levels of luteinising hormone. The egg is funneled into the Fallopian tube, and towards the uterus, by waves of small projections. The life span of the typical egg is quite short, only around 24 hours. Unless it meets a sperm on its journey within that time, it will die.
Luteal phase
During ovulation, the egg bursts from its follicle. However, the ruptured follicle remains on the surface of the ovary. For the next two weeks or so, the follicle transforms into a structure known as the corpus luteum. This structure starts releasing the sex hormone progesterone, along with small amounts of oestrogen. This hormonal combination maintains the thickened uterine lining, awaiting implantation of the fertilised egg. The corpus luteum needs the presence of an implanted fertilised egg (blastocyst) and its associated hormones (including human chorionic gonadotrophin) to continue producing elevated levels of progesterone and maintain the thickened uterine lining. If pregnancy doesn’t occur, the corpus luteum withers and dies, usually around day 22 in a 28-day cycle. The falling production of progesterone allows the uterine lining to come away. This is menstruation. The cycle then repeats.
Common menstrual problems
Some of the more common menstrual problems include:
- Premenstrual syndrome (PMS) - the activity of the corpus luteum and associated high levels of progesterone before a period can trigger a range of side effects in susceptible women including fluid retention, headaches, fatigue and irritability. Treatment options include exercise and dietary modifications.
- Dysmenorrhoea - or painful periods. It is thought that the uterus is prompted by certain hormones to squeeze far harder than necessary to dislodge its lining. Treatment options include painkillers.
- Menorrhagia - or heavy menstrual flow. Excessive periods can cause anaemia. Treatment options include oral contraceptives to regulate the flow.
- Amenorrhoea - or absence of the menstrual period. This is considered abnormal apart from pre-puberty, pregnancy, lactation and menopause. Possible causes include low body weight and excessive exercise.
Visitor
Labels
- Carcinoma (2)
- Dysmenorrhoea (4)
- Endometriosis (4)
- Female Genital Infection (3)
- Fluor Albus (4)
- General (3)
- Genital Prolapse (4)
- Gynecology (8)
- Infectious Disease in Pregnancy (13)
- Infertility (10)
- Menopause (3)
- Menstrual Disorder (10)
- Myoma Uteri (3)
- Obstetrics (13)
- Pelvic Floor (4)
- Pelvic Inflamatory Disease (3)
- Physiology of Human Reproductive System (4)
- Pregnancy (2)
- Sexually Transmitted Disease (6)
- Uterine Bleeding (4)
Followers
Facebook Badge
Copyright © 2009 Complicated Girl. All Rights Reserved.